Table of Contents

Hitting your 30s can feel like a bittersweet milestone. You are wiser, more confident, and likely juggling a whirlwind of responsibilities. But as life shifts gears, so does your body. This decade often marks the beginning of subtle changes in health — changes that, if caught early, can help you stay ahead of the curve for years to come. While it’s easy to get swept up in career goals, family life, or personal aspirations, taking a moment to prioritise your health can make all the difference.
Think of your 30s as the foundation-building phase for your long-term well-being. Just like you plan for the future in other aspects of life, regular health screenings are a proactive way to ensure your body is ready to support your ambitions. These screenings aren’t just about addressing current concerns — they are about prevention, early detection, and giving you peace of mind.
This guide provides an overview of the key health screenings to consider in your 30s, designed to help you prioritise your well-being.

1. General Health Screenings
As a doctor, one of the first things I tell my patients in their 30s is that this is the decade where prevention is key. Many health conditions, like hypertension, high cholesterol, and even diabetes, can develop silently during this time without any noticeable symptoms. That’s why regular health screenings are so crucial — they allow us to detect and address these issues early, often before they become serious.
When we talk about general health screenings, we are not just ticking boxes; we are creating a baseline for your health. For example, tests for blood pressure, cholesterol levels, and blood sugar help us identify risks for cardiovascular disease or diabetes. These are common conditions that, if caught early, can be managed effectively through lifestyle changes or medication.
Another thing to keep in mind is that your screening should be personalised. Family history, lifestyle factors, and even your work environment play a role in determining which tests are most relevant for you. For instance, if you have a family history of heart disease or diabetes, you should start screenings earlier or do them more frequently.
I always remind my patients that these check-ups aren’t just about finding problems — they are about creating a roadmap for better health. They give us a chance to talk about diet, exercise, and stress management, which are just as important as the numbers on a lab report.
2. Cardiovascular Health
In your 30s, I often notice patients starting to ask more questions about their heart health, and rightly so. This is the decade when the effects of years of habits — whether good or bad — begin to show. It’s not uncommon to see slightly elevated blood pressure or cholesterol levels during this time, often without any symptoms. That’s why I encourage regular check-ups and simple screenings to ensure we catch any changes early. These small steps can make a big difference in keeping your heart healthy and your future bright.
Blood Pressure Monitoring
Did you know high blood pressure, or hypertension, is often called the “silent killer”? ([1] It rarely shows symptoms until it has caused significant damage to your heart or other organs. Monitoring your blood pressure during routine check-ups can detect hypertension early, and allow timely intervention through lifestyle changes or medications. These simple screenings can prevent complications like heart disease or stroke.

Cholesterol Level Assessment
A lipid profile test is another essential screening in your 30s [2]. Elevated cholesterol, particularly LDL (bad cholesterol), can lead to plaque build-up in your arteries, which significantly increases the risk of heart attacks and strokes. If your cholesterol levels are higher than recommended, we can work together to develop a plan involving dietary changes, exercise routines, or medications to bring them under control.
Cardiac Screening Procedures at Ardennes Health
At Ardennes Health, we and our partner clinics offer a comprehensive range of cardiac screening procedures to evaluate your heart health thoroughly:
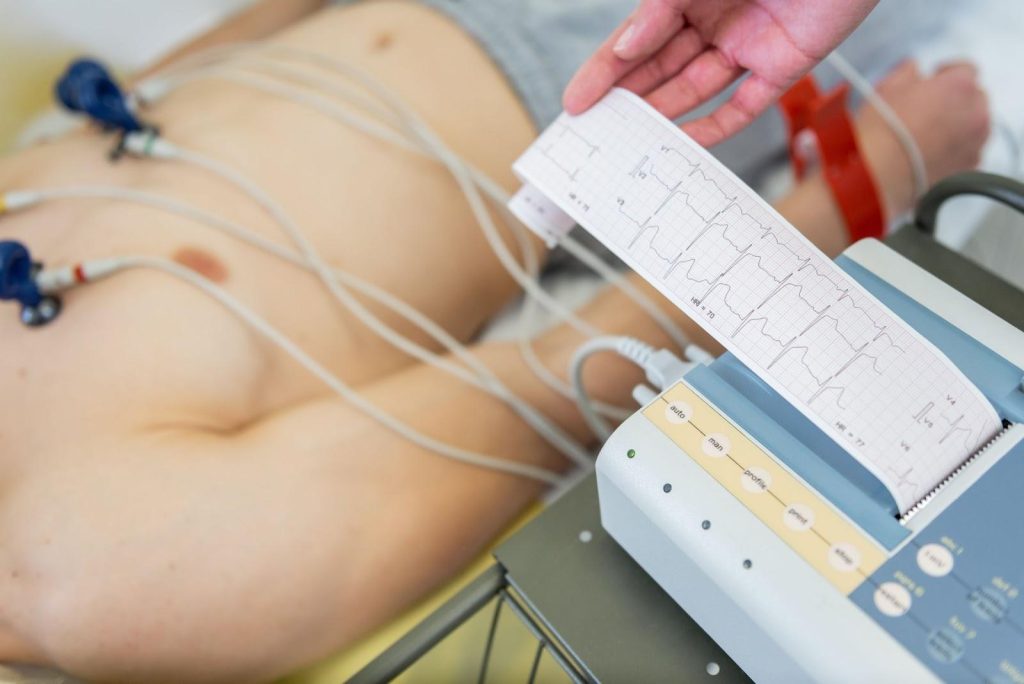
- Electrocardiogram (ECG): Records the heart’s electrical activity to detect conditions such as arrhythmias and ischaemia.
- Echocardiogram (ECHO): Provides detailed images of the heart’s structure and function, often used to assess the heart valves and chambers.
- 2D Echocardiography (2DE): Offers two-dimensional images of the heart, helping detect structural abnormalities.
- CT Angiogram: A non-invasive imaging test that visualises blood vessels to identify blockages or abnormalities in the arteries.
- Treadmill Exercise Test (TMX): Monitors heart activity during physical exertion to identify potential coronary artery diseases or other heart-related conditions.
Laboratory Investigations for Cardiac Risk
In addition to imaging tests, we recommend specific lab investigations to gain a comprehensive understanding of your cardiovascular health:
- Cardiac Risk Profile: Includes advanced markers like homocysteine, Apo A1, Apo B, and the Apo A1/B ratio [3].
- Diabetic Profile: Tests like HbA1c and fasting blood glucose to assess blood sugar levels, as diabetes is a significant risk factor for heart disease [4].
Whether you’re navigating a high-stress career, adjusting to parenthood, or simply working towards a healthier lifestyle, regular cardiac screenings are invaluable. These tests are not just for those with a family history of heart disease — they are for anyone who values their well-being. By prioritising these screenings now, you are building a solid foundation for a strong and healthy heart in the decades ahead.
3. Cancer Screenings
When it comes to cancer, early detection is your best defence. Many of my patients in their 30s ask whether it’s too soon to start thinking about cancer screenings. My answer is always the same: it’s never too early to prioritise your health, especially if you have a family history or other risk factors. Let me explain why these screenings matter and which ones you should consider.
Breast Cancer Screening
In your 30s, taking a proactive approach to breast health is essential, particularly if you have a family history of breast cancer or other risk factors. Routine mammograms are typically recommended starting at age 40 for women at average risk, but for those with a higher risk, earlier screenings may be necessary [5]. It’s always best to discuss your individual risk factors and screening plan with your healthcare provider.
For women in their 30s, breast ultrasounds can be a helpful option. This imaging technique uses sound waves to examine breast tissue and can detect abnormalities such as lumps or cysts. For those looking for additional and comprehensive screening methods, the Mastocheck Early Breast Cancer Screening is a valuable tool. This non-invasive blood test utilises proteomics-based early diagnostic technology to detect early-stage breast cancer. It’s particularly beneficial for women who may not yet need routine mammograms or who want an extra layer of reassurance.

Multi-Cancer Early Screening
Many people think cancer screenings are limited to specific types of cancer, but that’s no longer the case. With advancements in technology, we now have tests like LucenceINSIGHT that can screen for multiple cancers using a single blood sample. This test is a powerful tool for detecting cancers that are often asymptomatic in the early stages, such as pancreatic or ovarian cancer.
I recommend this test to anyone with a family history of cancer or to those who want a thorough evaluation of their health. LucenceINSIGHT helps us detect signals of cancer even when one is asymptomatic. This helps us detect issues early and act quickly, making it an excellent example of how modern medicine is transforming preventive care.
Cancer screenings aren’t about waiting for something to go wrong — they are about staying one step ahead. Whether it’s through a mammogram, Mastocheck, or LucenceINSIGHT, these tools help us identify risks early, giving you more options and better outcomes.
Summary
Entering your 30s is a turning point — a decade where proactive health choices can significantly shape your future well-being. By now, you have learned about the essential health screenings that address different aspects of your health: general health check-ups, cardiovascular assessments, and cancer screenings. But the key message is this: take action.
Health screenings aren’t just medical procedures; they are opportunities. Opportunities to catch silent health risks early, to make informed decisions, and to take preventive steps that can save you from future complications. This is your chance to build a foundation for a healthier, more resilient life — not just for yourself but for those who depend on you.
At Ardennes Health, we understand that taking the first step can sometimes feel overwhelming. That’s why we are here to make the process as efficient and supportive as possible. Whether it’s helping you choose the right screenings or guiding you through your results, our goal is to empower you to prioritise your health confidently. Schedule an appointment with us for your health screenings today.
References
- Research, C. for D. E. and. (2024). High blood pressure–understanding the silent killer. FDA. https://www.fda.gov/drugs/special-features/high-blood-pressure-understanding-silent-killer
- Lee, Y., & Siddiqui, W. J. (2025). Cholesterol levels. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK542294/
- Bodde, M. C., Hermans, M. P. J., Jukema, J. W., Schalij, M. J., Lijfering, W. M., Rosendaal, F. R., Romijn, F. P. H. T. M., Ruhaak, L. R., van der Laarse, A., & Cobbaert, C. M. (2019). Apolipoproteins A1, B, and apoB/apoA1 ratio are associated with first ST-segment elevation myocardial infarction but not with recurrent events during long-term follow-up. Clinical Research in Cardiology, 108(5), 520–538. https://doi.org/10.1007/s00392-018-1381-5
- Sherwani, S. I., Khan, H. A., Ekhzaimy, A., Masood, A., & Sakharkar, M. K. (2016). Significance of hba1c test in diagnosis and prognosis of diabetic patients. Biomarker Insights, 11, 95–104. https://doi.org/10.4137/BMI.S38440
- omlinson-Hansen, S. E., Budh, D. P., & Sapra, A. (2025). Breast cancer screening in the average-risk patient. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK556050/
Table of Contents
Health screenings are an important aspect of preventive healthcare, helping individuals detect potential issues early, manage existing conditions effectively, and maintain overall well-being. Health screenings are more than just routine check-ups—they are proactive steps toward a longer and healthier life.
In Singapore, common health issues include diabetes [1], cardiovascular diseases, and various types of cancer, several of which can be managed with early intervention. This guide will help you understand the types of health screenings that are relevant to you based on your age, gender, lifestyle, and risk factors.
Benefits of Regular Health Screenings
Regular screenings are vital for early detection and prevention. Beyond addressing physical health, these check-ups also provide peace of mind and the opportunity to make lifestyle changes and take better care of your health.
Here are some major benefits of regular health screenings:
- Early detection: Identifies diseases like diabetes, hypertension, or cancer before symptoms appear. This can improve the chances of successful treatment and recovery.
- Prevention of chronic health conditions: Health screenings enable timely intervention to prevent diseases from progressing into chronic conditions. It also helps people to understand their health and make lifestyle adjustments accordingly.
- Management of current conditions: Health screenings help individuals monitor their conditions and treatment so that they know they are taking the right steps, such as adjusting medications.
- Peace of mind and awareness: Regular health screenings help individuals alleviate their anxiety about perceived health problems and encourage proactive health management.

Health screenings, although general, are best tailored to each individual specifically depending on factors such as:
- Age
- Gender
- Family history
- Additional risk factors and concerns
This is why it’s important to book a consultation to evaluate each individual and their risk factors before recommending an appropriate health screening.
Health Screenings for Adults (General Recommendations)
Health screenings help adults stay ahead of health issues and challenges. Routine screenings give us valuable insights into our health and well-being, allowing us to detect and manage conditions such as high blood pressure and diabetes early. These tests offer a practical way to safeguard our health and make informed decisions.
Here are the general health screening recommendations for adults and their purposes:
- Blood Test: A general blood test assesses various components of the blood, such as red and white blood cell counts, haemoglobin, and platelets.
- Pressure Check: High blood pressure, or hypertension [2], is often called a “silent killer” because it usually presents no symptoms but significantly increases the risk of heart disease, stroke, and kidney failure. Regular blood pressure checks ensure early detection, allowing timely lifestyle changes or treatment to manage the condition and reduce long-term health risks.
- Cholesterol Test: A cholesterol test [3], or lipid profile, measures levels of good (HDL) and bad (LDL) cholesterol in the blood. High LDL or low HDL levels can lead to plaque buildup in arteries, increasing the risk of heart attacks and strokes. Regular monitoring helps to assess current cardiovascular health and encourages lifestyle and dietary changes.
- Blood Sugar Level Test: A blood sugar test evaluates glucose levels in the blood to detect prediabetes or diabetes. Early detection is critical for managing blood sugar and preventing complications such as nerve damage, kidney disease, and vision loss. Tests may include fasting blood sugar, HbA1c, or oral glucose tolerance tests.
- Body Mass Index (BMI) Measurement: The BMI test [4] measures body fat based on height and weight, indicating whether a person falls within a healthy weight range. It helps identify risks associated with obesity, such as diabetes, heart disease, and joint problems.
- Hepatitis Profile: This test screens for hepatitis viruses (A, B, and C), which can cause liver inflammation and damage.
- Renal Profile: The renal profile evaluates kidney function by measuring levels of creatinine, urea, and electrolytes like sodium and potassium in the blood. It also can detect kidney disease or dysfunction at an early stage.
- Thyroid Profile: This test measures thyroid hormone levels, including TSH, T3, and T4, to assess thyroid gland function and identify conditions like hypothyroidism or hyperthyroidism.
- Bone and joint screenings: Bone and joint screenings involve tests like bone density scans (DEXA) and assessments for inflammatory markers to evaluate bone strength and detect conditions like osteoporosis or arthritis.
- Tumor marker tests: These tests measure specific substances in the blood, urine, or tissues that may indicate the presence of certain types of cancer.
Preventive Cancer Screenings:
- Cervical Cancer: The Pap smear detects precancerous changes or abnormalities in the cervix, allowing early treatment before cancer develops. It is generally recommended for females aged 25-69.
- Breast Cancer: Mammograms use low-dose X-rays to detect breast cancer at an early stage before symptoms develop. Women aged 40 and older are recommended to undergo screenings every one to two years, depending on their risk factors and family history.
- Colorectal Cancer: Colorectal cancer screening involves tests like the faecal occult blood test (detecting hidden blood in stool) or colonoscopy (visual examination of the colon). These screenings identify early cancer or precancerous polyps.
- Prostate Cancer: The prostate-specific antigen (PSA) test measures PSA levels in the blood, which may indicate prostate cancer or other conditions like an enlarged prostate.
Other Essential Tests
- Liver and Kidney Function Tests: These blood tests evaluate the function of the liver and kidneys. They detect conditions like liver disease, hepatitis, or kidney damage, often before symptoms develop.
- Vision and Hearing Tests: Vision tests assess eye health and detect issues such as glaucoma, cataracts, or refractive errors. Hearing tests identify hearing loss, which is common with age or due to prolonged exposure to loud environments.

Health Screenings by Age
Health screenings are aligned with the specific needs of different age groups. In your 20s and 30s, baseline tests like blood pressure, cholesterol, and blood sugar assessments are typically recommended along with mental health screenings. In your 40s, more comprehensive screenings such as mammograms, Pap smears, and colonoscopies become crucial for detecting early signs of cancer. Women may also benefit from bone health assessments as hormonal changes begin to impact bone density.
In your 50s and beyond, screenings intensify to include heart health evaluations like stress tests and ECGs, as well as checks for dementia risk, vision, and hearing impairments. Tailoring screenings to your age ensures timely detection and intervention and contributes to more positive health outcomes.
Here are the recommended health screenings based on age groups:
| Age Group | Recommended Health Screenings |
| 30s – 40s | Cancer screenings (mammogram, Pap smear, colonoscopy)Bone health testsHormonal health checksSexually Transmitted Diseases (STD) checks |
| 40s – 50s | Cancer screenings (mammogram, Pap smear, colonoscopy)Bone health testsHormonal health checks |
| 50s and beyond | Frequent cancer screeningsHeart health tests (stress test, ECG)Dementia riskVision and hearing checks |
Health Screenings Based on Gender
Health screenings often vary by gender due to differences in anatomy, hormonal influences, and disease risks. While general tests such as blood tests and cholesterol checks are the same recommendations for both genders, other tests differ. For women, screenings often include reproductive and hormonal health, including Pap smears [5] for cervical cancer, mammograms for breast cancer, and bone density tests to monitor osteoporosis risk, particularly after menopause.
For men, health screenings may also include prostate cancer screenings (PSA tests) [6] and guidance on testicular self-examinations to help detect specific cancers early. Gender-specific screenings provide a comprehensive approach to maintaining health and addressing risks effectively.
Here are some recommended health screenings based on gender:
| Gender | Recommended Health Screenings |
| Women | Cervical Cancer Screening (Regular Pap smears)Breast Cancer Screening (Mammograms starting at age 40)Bone density testsPregnancy-related screeningsHormonal checks |
| Men | Prostate Cancer Screening (Men aged 50 and above).Cardiovascular Health CheckHormonal checks |

Health Screenings Based on Lifestyle, Risk Factors, and Specific Conditions
Your lifestyle and personal risk factors also influence the type of health screenings you need. Smokers, for example, should prioritise lung cancer screenings and respiratory function tests to detect potential damage early. If you have a family history of chronic diseases such as diabetes, heart disease, or cancer, genetic testing and enhanced cancer screenings can provide important insights. Sedentary lifestyles increase the risk of cardiovascular diseases and diabetes, making ECGs, stress tests, and blood sugar screenings essential.
If you already have a specific condition, you may also require additional health screenings. Here are some health screenings based on lifestyle and risk factors that you should consider:
| Lifestyle/Risk Factors | Recommended Health Screenings |
| Smokers | Lung cancer screeningRespiratory function testsCardiovascular health checkGeneral health screening |
| Family history of chronic diseases | Cancer screeningsCardiovascular health checkDiabetes screeningBone health assessmentGeneral health screening Kidney function test |
| Sedentary | Cardiovascular health checkGeneral health screeningMusculoskeletal assessmentsMental health screeningLiver and kidney function test |
| Specific condition | Chronic Illnesses: Lipid profile test Kidney Function tests Blood pressureDiabetes testLiver function testThyroid profile Heart Disease and Stroke Risk: ECG testEchocardiogramCholesterol levelsCT AngiogramLipoprotein(a)Homocysteine |

How to Choose a Health Screening Package in Singapore
Selecting the right health screening package in Singapore depends on your individual needs, budget, and preferences.
Private screening packages are also available for those seeking more comprehensive or personalised care. When choosing a private package, consider factors like the clinic’s reputation, the details of the tests included, and overall value for money. If you aren’t sure which health screening you should undergo, book a consultation with a doctor.
At Ardennes Health, we offer comprehensive health screening packages tailored to your needs and follow-up consultations to address any findings. Whether it’s preventive care or managing an existing condition, our team is here to guide you every step of the way.
Book your health screening with us at Ardennes Health or check out our packages here.
When to Seek Specialist Care
If your health screening results indicate abnormal findings, it’s important to seek medical advice as soon as possible. Abnormal results may signal underlying conditions that require further investigation. Based on the findings, your doctor may refer you to a specialist for a more in-depth evaluation and treatment. For example, if your screening suggests potential cancer, you may be referred to an oncologist, while abnormal heart test results may lead to a consultation with a cardiologist. Early intervention is crucial for managing health conditions effectively and improving long-term outcomes.
Conclusion
Regular health screenings are essential for everyone to stay aware of long-term health and proactive management of potential issues. Take charge of your health today by scheduling screenings tailored to your needs. If you’re still unsure which screening you should book, consult with our doctors to identify the most suitable options for you.
Frequently Asked Questions
What are the most important health screenings?
For most adults, important health screenings include body mass index (BMI), cholesterol and blood pressure screening, kidney function tests, tumour markers, and more. However, it depends on the individual and their lifestyle, age, and gender.
How often should I do health screening in Singapore?
The frequency of a health screening depends on various factors, including your age, gender, family history, and overall health status. For most adults, scheduling a comprehensive health screening every one to two years is an ideal approach to maintaining well-being. Consult with your doctor for more information.
Is health screening the same as medical check-up?
No, they are related but different. Health screenings are specific tests based on age, gender, or risk factors, while a medical check-up is a general examination by a doctor. Screenings are an important aspect of check-ups and help doctors gain a comprehensive understanding of your health to determine treatment or lifestyle changes.
References
- Channel NewsAsia. (2023, November 17). War against diabetes: Doctors seeing rise in patients below 40 due to lifestyle habits, early screening. Channel NewsAsia. Retrieved from: https://www.channelnewsasia.com/singapore/war-against-diabetes-singapore-doctors-seeing-rise-young-patients-below-40-lifestyle-habits-stress-early-screening-treatment-3921976
- Mayo Clinic. (n.d.). High blood pressure (hypertension) – Symptoms and causes. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/syc-20373410
- Cleveland Clinic. (n.d.). Cholesterol: Understanding levels & numbers. Cleveland Clinic. Retrieved from: https://my.clevelandclinic.org/health/articles/11920-cholesterol-numbers-what-do-they-mean
- Singapore Heart Foundation. (n.d.). BMI calculator. Singapore Heart Foundation. Retrieved from https://www.myheart.org.sg/tools-resources/bmi-calculator/
- Mayo Clinic. (n.d.). Pap smear: Overview. Mayo Clinic. Retrieved from https://www.mayoclinic.org/tests-procedures/pap-smear/about/pac-20394841
- Singapore Cancer Society. (n.d.). Prostate cancer. Singapore Cancer Society. Retrieved from https://www.singaporecancersociety.org.sg/learn-about-cancer/types-of-cancer/prostate-cancer.html
- Ministry of Health Singapore. (2024, December 2). Community Health Assist Scheme (CHAS). Ministry of Health. Retrieved from https://www.moh.gov.sg/managing-expenses/schemes-and-subsidies/chas
- Ministry of Health Singapore. (2024, December 2). Enhanced Screen for Life. Ministry of Health. Retrieved from https://www.moh.gov.sg/managing-expenses/schemes-and-subsidies/enhanced-screen-for-life
Breast cancer remains a significant health concern for women throughout the globe. In Singapore, it stands as the most common type of cancer among women. The Singapore Cancer Registry [1] reported that breast cancer accounts for nearly one in three cancer diagnoses among women in the country. This translates to 29.7% [2] of all female cancers, with approximately 1,100 new cases diagnosed annually. However, what is even more concerning is the fact that roughly 270 women [3] succumb to the disease each year.
Due to its prevalence, early detection through regular screening plays a critical role in improving the survival rate. In fact, research shows that early diagnosis can increase the chances of successful treatment by as much as 90% [4].
The aim of breast cancer screening is to identify the cancer at its earliest stage, ideally before symptoms are noticeable. By detecting cancer early, women have more treatment options available, and a greater likelihood of successful outcomes. This guide will provide a comprehensive overview of the breast cancer screening options available today, from blood tests to mammograms, and how each method can contribute to early detection.

Understanding Breast Cancer Screening
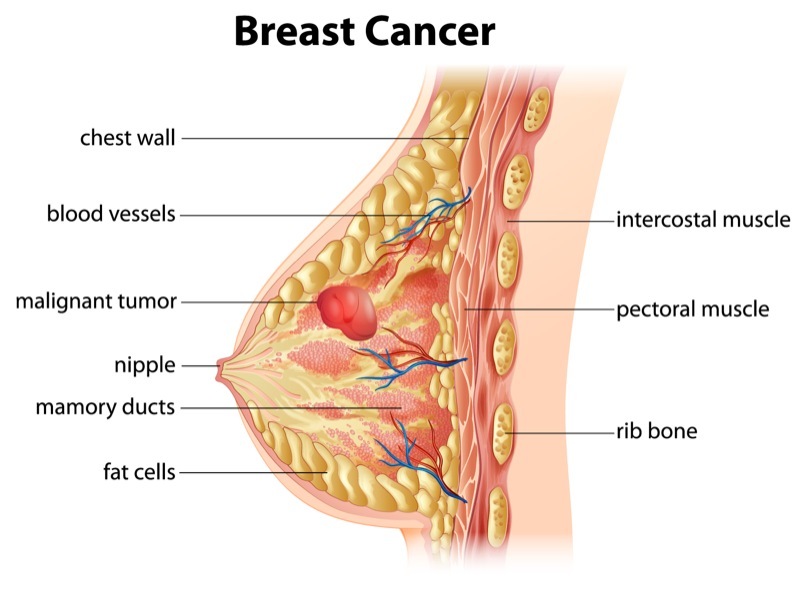
Breast cancer screening refers to the preventive measures taken to detect breast cancer before any symptoms emerge. Unlike diagnostic tests that are performed when there are visible signs, or symptoms of breast cancer, screening is done on seemingly healthy individuals, especially among those with a family history of breast cancer. The primary objective of screening is to identify cancer early, ideally when it is confined to the breast tissue, and has not spread to other parts of the body.
Regular breast cancer screening is essential for all women, particularly those over the age of 40 years old, or those with a family history of breast cancer. However, women with other high-risk factors as listed below may need to begin screening early:
- Age — as women age, the risk of breast cancer increases, with most cases diagnosed after the age of 50 [5].
- Dense breast — women with dense breasts [6] are more at risk of breast cancer, with the density making it harder to see tumours on a mammogram.
- Family history — a family history [8] of breast cancer increases the possibility of breast cancer.
- Genetics — inherited mutations to certain genes (BRCA1, and BRCA2 [9]) can increase the likelihood of developing breast cancer.
- Menstrual history — women who started menstruating before 12 years old, or started menopause after 55 years old are more at risk of developing breast cancer due to the long exposure to hormones [11].
- Previous breast cancer history — women with a previous history of breast cancer [12] are at risk of relapsing. Meanwhile, women with a history of benign breast diseases like lobular carcinoma in situ, or atypical ductal hyperplasia, are more prone to developing breast cancer.
- Previous radiation treatment — prior exposure to radiation [13] due to treatment to the chest, or breasts before 30 years old increases the risk of breast cancer.
- Alcohol consumption — a woman’s risk of developing breast cancer increases if she consumes alcohol at an excessive rate [14].
- Lifestyle — women who lead a sedentary, or not physically active lifestyle are at an increased risk of developing breast cancer.
- Weight — women who are considered overweight or obese [15] after going through menopause are more likely to develop breast cancer compared to those who maintain a healthy weight.

It is important to understand that consistent screening can significantly improve a woman’s chance of beating the cancer, as early detection may also include the following benefits:
- Early intervention and treatment
- More treatment options available
- Better outcomes and results
- Lowers the necessity for more aggressive treatments
- Higher quality of life post-recovery
- Reduces the mortality rate
Be that as it may, it is crucial to choose the appropriate screening method based on individual risk factors, age, and lifestyle. In fact, working closely with a licensed, and qualified medical practitioner will be advantageous, as they can help tailor a screening plan that best suits each woman’s needs.
Breast Cancer Screening Methods
There are various screening methods available today, each with its own unique benefits, and limitations. These include blood tests, imaging techniques like mammograms, ultrasounds, and magnetic resonance imaging (MRI) for those at high risk. While there are many options available, the choice of screening method often depends on the individual’s risk profile, and medical history. The following briefly describes each method:
- Self examination — self examination involves checking your own breasts for lumps, changes in breast size or shape, nipple discharge or discolouration.
- Clinical breast exams — clinical examinations are performed by a trained doctor, who will check for breast abnormalities or lumps.
- Blood tests — Conventional blood tests can be undergone to detect breast cancer markers, as well as innovative advancements, such as Mastocheck (link to service page), which identifies specific biomarkers linked to early-stage breast cancer for earlier detection.
- Imaging tests — Imaging tests, such as mammograms, ultrasounds and magnetic resonance imaging (MRIs).
Each method plays a different role in breast cancer detection, and often, a combination of these tests may be necessary for comprehensive screening.
Blood Tests

Blood tests are often used to detect early signs of breast cancer. These tests work by identifying specific proteins, or markers, that cancer cells release into the bloodstream. To give an example, markers like CA 15-3, and CEA can sometimes indicate the presence of cancer, although these markers are not exclusively specific to breast cancer.
Even so, blood tests are valued for their non-invasive nature. They can be conducted quickly, with results available in a shorter time frame compared to imaging techniques. However, while blood tests can provide valuable information, they are not typically used as standalone diagnostic tools. Their sensitivity, and specificity are limited, meaning that they are better suited as supplementary tests rather than primary screening tools.
That being said, blood tests are particularly useful for monitoring patients who have already been diagnosed with cancer to track the effectiveness of treatment, or detect recurrences. Be that as it may, as a screening tool, blood tests should be paired with other methods like imaging for a more accurate diagnosis.
The Role of Mastocheck in Early Screening
At Ardennes Healthcare, our Mastocheck Early Breast Cancer Screening (link to service page) is a blood test that analyses specific protein biomarkers that are indicative of breast cancer.
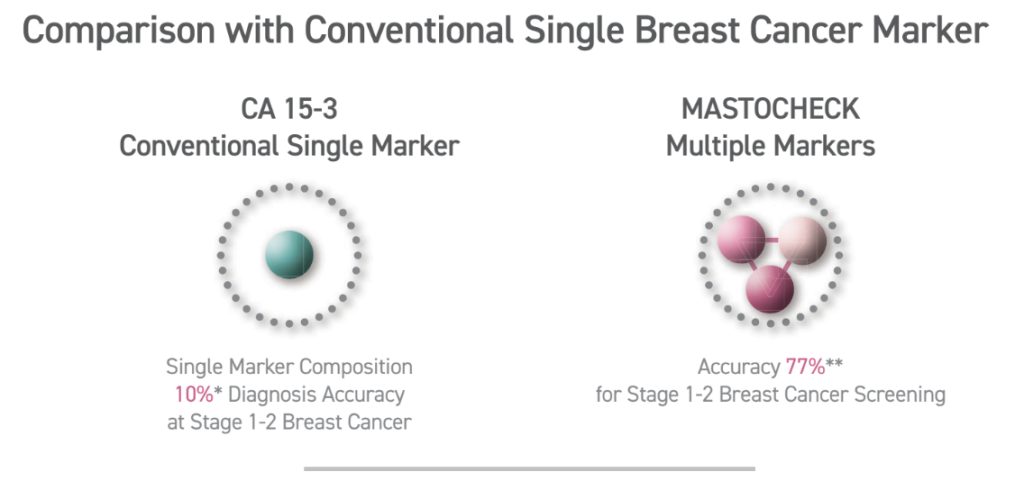
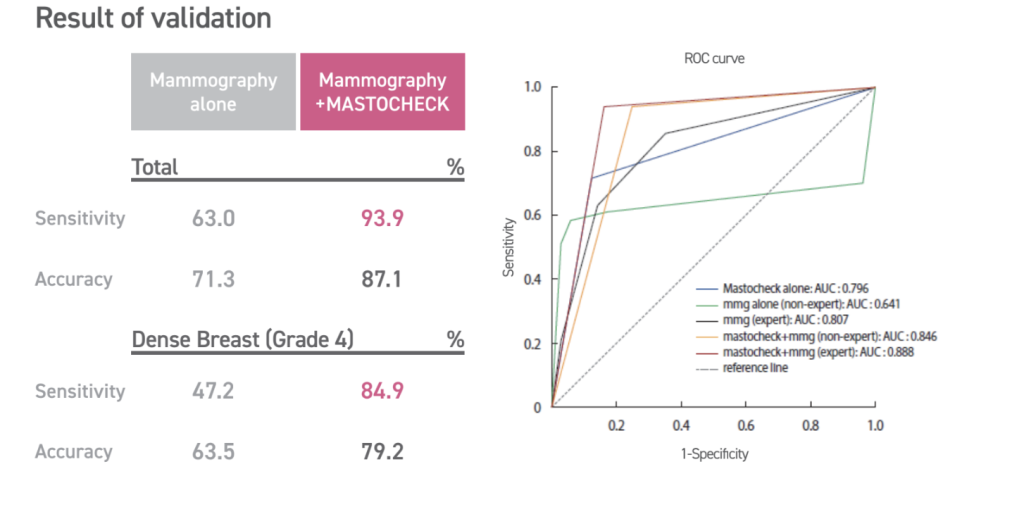
Unlike traditional blood tests that focus solely on inherited mutations, Mastocheck utilises advanced proteomic analysis to identify tumour-related proteins which are released by cancer cells and can serve as early indicators of tumour presence. This test is non-invasive, requiring only a blood sample, and can identify cancerous changes (disease-specific expression patterns) before they become visible through imaging. Hence, proteomics-based early diagnosis technology, like Mastocheck, greatly maximises diagnostic accuracy — with about 77% accuracy for stage 1-2 breast cancer.
However, it is essential to understand that while various blood tests can provide valuable insights into cancer risk, it is not a replacement for imaging techniques. Rather, it serves as a complementary tool, especially for those at higher risk of cancer (shows 10%-30% higher sensitivity compared to Mammography alone). Knowing your current cancer status through Mastocheck can help navigate the decision-making process regarding the frequency of follow-up screenings or the need for further diagnostic imaging.
The benefits of Mastocheck
The benefits of Mastocheck screening include:
- Early detection — Mastocheck enables the identification of breast cancer in its earliest stages, even before it becomes detectable through conventional imaging methods.
- Non-invasive procedure — Mastocheck only requires a small blood sample, offering a stress-free and comfortable screening process.
- High accuracy — It utilises advanced molecular diagnostic techniques, which allows it to detect specific cancer-related biomarkers, ensuring precise and reliable results.
- Enhanced detection for dense breasts — Mastocheck is especially effective for women with dense breast tissue where traditional mammograms may fall short in detecting. It delivers 10% – 30% greater sensitivity compared to a mammogram alone.
- Optimised outcomes — Early detection with Mastocheck increases the likelihood of successful treatment outcomes and reduces the need for more aggressive treatments.
- Radiation-free — By detecting cancer biomarkers without using radiation, Mastocheck provides a safer alternative for breast cancer screening.
- Accessibility — Suitable for younger women (ages 20 – 40), pregnant women, and those with breast implants or dense breast tissue.
Mammograms

Mammograms (link to service page) remain one of the most reliable screening tools for early breast cancer detection. This method involves using low-dose X-rays to examine breast tissue for any signs of tumours, or abnormal growths. For women aged 40, and above, regular mammograms are often recommended, as the risk of developing breast cancer increases with age.
A screening mammogram is typically done once every one to two years for women at average risk, while those at higher risk may need to undergo mammograms more frequently.
The benefits of mammograms are well-documented. In fact, they have been shown to reduce breast cancer mortality by enabling earlier diagnosis. However, some women may find the procedure uncomfortable due to the compression of breast tissue required for clear imaging. Additionally, mammograms do expose women to a small amount of radiation, but the risk is generally outweighed by the benefits of early detection.
Ultrasound and MRI: Complementary Tools

While mammograms are effective for most women, certain cases may require additional imaging techniques, like ultrasounds, and MRIs.
Ultrasound imaging (link to service page) is particularly useful for women with dense breast tissue, where mammograms may not be as effective. Dense tissue can obscure tumours, making them harder to detect. Ultrasound also works using sound waves to create images of the breast tissues, allowing for better visualisation of abnormalities that may not appear on a mammogram.
Meanwhile, MRI is an advanced imaging technique, typically for high-risk individuals. MRIs use magnetic fields, and radio waves to create detailed images of the breast, making it possible to detect cancers that might be missed by mammograms, or ultrasounds. In fact, women with a strong family history of breast cancer, or those with known genetic mutations like BRCA1, or BRCA2 may benefit from regular MRIs in addition to mammograms.
Both ultrasounds and MRIs serve as complementary tools to mammograms, and are usually recommended when additional clarity is needed.
A comprehensive approach: Mammogram with Mastocheck
The importance of early detection in breast cancer
Early detection of breast cancer greatly improves survival rates and treatment outcomes. In fact, there is a 5-year relative survival rate for localised (tumour is confined to breast tissue) breast cancer is approximately 99%. This makes early detection of breast cancer and timely treatment paramount.
Why combine Mammogram and Mastocheck?
- Mastocheck — Mastocheck is a blood-based test that detects specific biomarkers linked to breast cancer, and offers 77% accuracy for stage 1-2 breast cancer screening. In contrast, conventional single marker CA15-3 offers an accuracy of 10%. In comparison, Mastocheck has a higher sensitivity and more accuracy in early-stage detection.
- Mammogram — A Mammogram is a widely used imaging test that plays an important role in breast cancer detection, and is highly effective at visualising microcalcifications and small masses and tumours in the breast that can indicate early-stage cancers. This makes it a reliable, non-invasive way to detect cancer early and improve treatment outcomes.
Combining a Mammogram with Mastocheck allows your doctor to detect structural changes in breast tissue and molecular changes in biomarkers that indicate early-stage breast cancer, offering a comprehensive significantly reducing the chances of false negatives.
Undergoing a Mastocheck blood test can also reduce your need for unnecessary procedures and additional stress. This is because it provides additional confirmation when ambiguous findings are detected via the mammogram, helping differentiate between the benign and malignant abnormalities in the breast.
What to Expect During a Breast Cancer Screening
We understand that undergoing breast cancer can be a daunting experience. At Ardennes Healthcare, we strive to help alleviate anxiety, and ensure you are well-prepared. Here, we break down the step-by-step for our general breast cancer screening procedures that are available at our healthcare facility.
Initial Consultation and Pre-Screening Assessment
Your breast cancer screening journey typically begins with an initial consultation with our general physician. During the consultation, our doctor will review your medical history, including any personal, or family history of breast cancer. They may ask about your lifestyle, any current symptoms you are experiencing, and other risk factors that may impact your screening plan. This consultation is essential as it ensures that the screening method chosen is appropriate for your specific risk profile.
Blood Tests (if applicable)
For those opting for blood tests like the Mastocheck screening, the procedure is straightforward and quick. Our nurse will draw a blood sample from a vein in your arm. The process typically takes less than 10 minutes, and is relatively painless, with only a minor prick sensation. The sample is then sent to a laboratory for analysis to detect potential cancer markers. While you are permitted to go home immediately after the procedure is done, results are generally available within a few days to a week.
Mammogram
If your screening includes a mammogram, you will be asked to change into a hospital gown, and remove any jewellery or clothing above the waist. Our technician will then position your breast on a flat surface, and gently compress it with a clear plastic plate. This compression is necessary to get a clear image of the breast tissue, and may cause some discomfort, but it only lasts for a few seconds. The technician will take images from different angles, usually two per breast. A simple mammogram process takes about 20 minutes to complete.
After the imaging is complete, the radiologist will review the images for any signs of abnormalities. It may take a few days for you to receive your results. In the event any suspicious findings are detected, further diagnostic tests may be recommended.
Ultrasound
For women with dense breast tissue, or if additional imaging is needed, an ultrasound may be recommended. During an ultrasound, you will lie down while a technician applies a gel to your breast. A handheld device called a transducer is moved over the area to capture images using sound waves. This procedure is painless and takes about 15 to 30 minutes.
Post-Screening Consultation
Once all of the tests are completed, you may have a follow-up consultation to discuss the results. If abnormalities are found, our doctor provider will guide you through the next steps, which may include additional diagnostic tests, biopsies, or further imaging to confirm the presence of cancer.

How to Prepare for Breast Cancer Screening
Being well-prepared can help ensure a smooth, and effective screening experience. To help you prepare for your breast screening, here is a detailed guideline to get you started.
Step 1: Scheduling Your Appointment
When scheduling an appointment for breast screening, do remember to pick a date at least a week after your menstrual period. This is due to the fact that your breasts are less likely to be tender during this time. Doing so can help minimise discomfort during the procedure. Additionally, for women undergoing blood tests or other non-imaging tests, there are no specific timing requirements.
Step 2: Dress Comfortably
On the day of your screening, wear a two-piece outfit so that you can easily remove your top piece of clothing for imaging procedures. Avoid wearing deodorant, antiperspirant, powders, or lotions on your underarms or breasts, as these products can show up on mammogram images as white spots, potentially leading to false alarms.
Step 3: What to Bring
It is important to bring your identification, health insurance information, and any prior imaging results if you have been screened before. Having these past records allows our doctors, and radiologists to compare images, and detect any subtle changes in breast tissue over time.
Step 4: Pain Management
If you are concerned about discomfort during a mammogram, consider taking an over-the-counter pain reliever, such as ibuprofen or acetaminophen, about an hour before your appointment. This can help alleviate any pain associated with breast compression. However, always speak with your doctor before taking any medication to prevent any complications.
Step 5: Preparing for an MRI
If you are scheduled for an MRI, inform the technician if you have any metal implants, pacemakers, or allergies, particularly to contrast dyes. You may need to fast for a few hours before the test if a contrast dye is being used. Additionally, do remember to remove any metal objects, such as jewellery, belts, or watches, before the scan, as this can disrupt the imaging process.
Step 6: Mental Preparation
For some women, the thought of undergoing a breast cancer screening can be anxiety-inducing, especially if it is their first time. But do remind yourself that these screenings are proactive steps toward maintaining your health, rather than dwelling on the possibility of malignancy. Some tips that can help ease your nerves before your appointment include deep breathing exercises, or listening to calming music. In fact, if asking questions can help reduce your anxiety, then do feel free to speak with our doctors to help you be more mentally prepared for the screening.
Step 7: Post-Screening Care
After your screening, there are generally no restrictions, and you can resume your normal activities immediately. However, if you experience any soreness after a mammogram, applying a cold compress can help reduce discomfort. For blood tests, keep the bandage on for a few hours to avoid bruises.
By following these preparation steps, and understanding what to expect, you can make your breast cancer screening experience as comfortable, and stress-free as possible.

Breast Cancer Screening Methods & Cost at a Glance
| Feature | Mammogram | Ultrasound | Mastocheck |
| Purpose | Standard screening for breast cancer. | Complements mammograms and can be used to evaluate dense breast tissue. | Blood test for early detection of specific biomarkers for breast cancer. |
| Recommended for | Women over the age of 40 years old or have risk factors for breast cancer. | Women with dense breasts, palpable lumps or other possible breast cancer indicators. | Early detection or supplemental screening. |
| Technology | X-ray imaging, may sometimes include a contrast for Contrast Enhanced Mammogram (CEM). | Utilises targeted ultrasound waves to visualise breast tissue structures. | Blood sample analysed for cancer markers. |
| Sensitivity | High sensitivity, but may not be as effective for dense breast tissue | High sensitivity, but may miss small or early cancers. | High sensitivity and provides risk indication for early cancers, but not the specific tumour location. Good early-warning tool. |
| Radiation exposure | Low-dose radiation. | None. | None. |
| Cost | From $99 | From $140 | From $170 |
Take Charge of Your Breast Health Today
Breast cancer screening is a powerful tool that can save lives by catching cancer early, often before any symptoms appear. However, deciding on the right screening plan is a highly personalised process that takes into account factors such as age, family history, genetic predisposition, and lifestyle. Understanding your options empowers you to make informed decisions about your health, and overall well-being.
For women in their 40s, annual mammograms are often recommended. However, younger women with elevated risk factors may benefit from additional testing options, such as Mastocheck, or breast ultrasounds. It goes without saying that consulting with a licensed, experienced physician is essential to developing a sound screening strategy tailored to your specific needs. A personalised plan not only maximises the effectiveness of early detection, but also offers peace of mind, knowing that you are taking proactive steps to protect your health.
At Ardennes Healthcare, we are dedicated to empowering women with comprehensive breast health services. We offer advanced screening options, including the Mastocheck test, to ensure you receive the best possible care. Our team is committed to providing personalised guidance every step of the way, helping you achieve optimal outcomes.
Remember, early detection is key. Take control of your breast health today! Schedule your screening appointment (link to contact us page) with us, and embark on a proactive journey toward wellness.
References
[1] Breast Cancer. (n.d.). In www.singaporecancersociety.org.sg. Retrieved November 14, 2024, from https://www.singaporecancersociety.org.sg/learn-about-cancer/types-of-cancer/breast-cancer.html
[2] [3] Jara-Lazaro, A. R., Thilagaratnam, S., & Tan, P. H. (2010). Breast cancer in Singapore: some perspectives. In Breast cancer (Tokyo, Japan) (Vol. 17, Issue 1, pp. 23–28). Breast cancer (Tokyo, Japan). https://doi.org/10.1007/s12282-009-0155-3
[4] By. (n.d.). The landscape of breast cancer screening and treatment in Singapore. In how well do we know it. Retrieved November 14, 2024, from https://www.singhealth.com.sg/news/medical-news-singhealth/landscape-breast-cancer-screening-treatment-singapore
[5] CDC. (2024). Breast Cancer Risk Factors. In Breast Cancer. https://www.cdc.gov/breast-cancer/risk-factors/index.html
[6] Dense Breasts: Answers to Commonly Asked Questions – NCI. (2018). In www.cancer.gov. https://www.cancer.gov/types/breast/breast-changes/dense-breasts
[7] Diethylstilbestrol (DES) Exposure and Cancer – NCI. (2021). In www.cancer.gov. https://www.cancer.gov/about-cancer/causes-prevention/risk/hormones/des-fact-sheet
[8] Brewer, H. R., Jones, M. E., Schoemaker, M. J., Ashworth, A., & Swerdlow, A. J. (2017). Family history and risk of breast cancer: an analysis accounting for family structure. In Breast cancer research and treatment (Vol. 165, Issue 1, pp. 193–200). Breast cancer research and treatment. https://doi.org/10.1007/s10549-017-4325-2
[9] Petrucelli N, Daly MB, Pal T. BRCA1- and BRCA2-Associated Hereditary Breast and Ovarian Cancer. 1998 Sep 4 [Updated 2023 Sep 21]. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1247/
[10] Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Collaborative Group on Hormonal Factors in Breast Cancer. (1997). Lancet (London, England), 350(9084), 1047–1059.
[11] Eaton L. (2002). Early periods and late childbearing increase risk of breast cancer, study confirms. BMJ : British Medical Journal, 324(7334), 386.
[12] Zeinomar, N., Phillips, K. A., Daly, M. B., Milne, R. L., Dite, G. S., MacInnis, R. J., Liao, Y., Kehm, R. D., Knight, J. A., Southey, M. C., Chung, W. K., Giles, G. G., McLachlan, S. A., Friedlander, M. L., Weideman, P. C., Glendon, G., Nesci, S., kConFab Investigators, Andrulis, I. L., Buys, S. S., … Terry, M. B. (2019). Benign breast disease increases breast cancer risk independent of underlying familial risk profile: Findings from a Prospective Family Study Cohort. International journal of cancer, 145(2), 370–379. https://doi.org/10.1002/ijc.32112
[13] Joshi, S. C., Khan, F. A., Pant, I., & Shukla, A. (2007). Role of radiotherapy in early breast cancer: an overview. International journal of health sciences, 1(2), 259–264.
[14] Liu, Y., Nguyen, N., & Colditz, G. A. (2015). Links between alcohol consumption and breast cancer: a look at the evidence. Women’s health (London, England), 11(1), 65–77. https://doi.org/10.2217/whe.14.62
[15] Dehesh, T., Fadaghi, S., Seyedi, M., Abolhadi, E., Ilaghi, M., Shams, P., Ajam, F., Mosleh-Shirazi, M. A., & Dehesh, P. (2023). The relation between obesity and breast cancer risk in women by considering menstruation status and geographical variations: a systematic review and meta-analysis. BMC women’s health, 23(1), 392. https://doi.org/10.1186/s12905-023-02543-5

