
Turning 50 years old is a milestone worth celebrating, but it is also a good time to start taking health checks more seriously. As we age, our risk of chronic illnesses rises and many conditions can develop silently without obvious symptoms. Health screening enables seniors to identify problems early, when treatment is more effective and recovery outcomes are better.
In Singapore, where life expectancy is among the highest in the world, regular health screening after 50 years old plays a vital role in maintaining independence and enjoying a good quality of life.
Why Health Screening Matters After 50
From the age of 50 onwards, the body becomes more vulnerable [1] to conditions such as heart disease, diabetes, osteoporosis and cancer. These illnesses often progress quietly in the background and may only show symptoms when they have already advanced. By the time signs appear, treatment can become more complex and recovery more challenging. Regular health screening bridges this gap, uncovering health issues in their early stages when they are easier to treat and sometimes even preventable.
Singapore’s Ministry of Health (MOH) also encourages preventive care through national initiatives [2], such as the Healthier SG programme, which makes screenings accessible and affordable. This approach reflects a broader commitment to promoting healthy ageing, helping seniors maintain independence and quality of life for as long as possible. Beyond detecting illness, health screening also offers reassurance, guiding lifestyle choices and motivating individuals to stay active and well.
With this in mind, what exactly should seniors focus on once they reach 50 years old? This guide will walk you through the core tests that help monitor important aspects of health and detect conditions that often become more common with age.
General Health Screening Tests Recommended After 50

Health screening after 50 years old is not about finding problems for the sake of it. Rather, it is about building a clearer picture of one’s health and identifying risk factors early. The tests recommended at this stage of life are designed to cover the body’s major systems, which include cardiovascular, metabolic, digestive, skeletal and sensory. These systems are more prone to age-related changes.
Each test plays a role in detecting silent conditions that may otherwise go unnoticed until they cause significant harm. By keeping track of these key areas, seniors can take timely steps to protect their health and make informed decisions about treatment and lifestyle.
Blood Pressure and Cholesterol Check
Cardiovascular disease remains one of the leading causes [3] of illness and death among seniors in Singapore. High blood pressure and elevated cholesterol levels often exhibit no noticeable signs but quietly strain the heart and blood vessels. Regular checks allow doctors to detect hypertension or unhealthy lipid profiles early. With guidance, seniors can manage these risks through lifestyle adjustments such as improved diet and exercise, or through medication if needed, reducing the likelihood of a heart attack or stroke.
Blood Sugar Test (Diabetes Screening)
Diabetes is sometimes called a silent disease because many people have it for years without realising it. In Singapore, its prevalence rises steeply with age [4], and poorly controlled diabetes can lead to complications such as kidney disease, nerve damage and vision loss. A fasting blood sugar test or HbA1c test helps identify diabetes or prediabetes, providing seniors with the opportunity to intervene early and prevent complications before they set in.
Kidney and Liver Function Tests
The kidneys and liver play vital roles in filtering waste, balancing body chemistry and processing nutrients and medications. As such, problems with these organs often develop silently and may only be discovered when damage is significant. Simple blood tests can evaluate kidney function by measuring creatinine and the glomerular filtration rate, while liver tests examine enzymes and proteins that signal how well the organ is working. These checks are essential for seniors with diabetes, high blood pressure, or a history of alcohol use.
Cancer Screening
Cancer risk increases with 5] age, and screening helps to detect certain types of cancer early, when treatment is most effective. To get ahead of the disease, there are several recommended targeted screenings, such as:
- Colorectal cancer – both men and women aged 50 years old should undergo regular checks, either with a Faecal Immunochemical Test (FIT) annually or a colonoscopy every 10 years.
- Breast cancer – women between 50 and 69 years old are advised to have a mammogram every two years.
- Cervical cancer – screening with Pap smears or HPV testing remains important for women up to the age of 65 years old.
- Prostate cancer – men over 50 years old should discuss with their doctor whether the PSA test is suitable, particularly if there is a family history of the disease.
These screenings are tailored to the most common cancers affecting older adults in Singapore, providing peace of mind while increasing the chance of successful treatment.
Bone Health Screening (Osteoporosis Test)
Bones naturally lose density with age [6], making them more fragile and prone to fractures. This risk is even greater in women after menopause due to hormonal changes. A bone mineral density scan (DEXA scan) can identify osteoporosis before fractures occur, allowing preventive treatment such as calcium and vitamin D supplementation, exercise programmes and medication if required. It is important to understand that protecting bone health is crucial for reducing the risk of falls and maintaining mobility in later years.
Eye and Hearing Tests
Changes in vision [7] and hearing are often gradual and easily overlooked, yet they can significantly impact safety, communication and independence. Eye examinations help detect cataracts, glaucoma and macular degeneration, all of which become more common with age. Early intervention preserves vision and prevents avoidable blindness. Meanwhile, hearing assessments are equally important, as untreated hearing loss [8] can contribute to social withdrawal, falls and even cognitive decline. The timely use of aids or treatment supports a better quality of life and daily functioning.
Optional but Valuable Health Checks for Seniors

Beyond the essential tests, there are additional screenings that may not be mandatory but can provide valuable insights into a senior’s overall well-being. These checks help identify subtler issues that may affect energy levels, mood, memory and long-term health. While they may not be needed for everyone, discussing them with a doctor can help seniors decide whether they would be beneficial based on personal risk factors and medical history.
Vitamin D and B12 Levels
Deficiencies in these vitamins are more common in older adults, partly due to changes in diet and the body’s reduced ability to absorb nutrients efficiently with age. Low vitamin D [9] can weaken bones and increase the risk of fractures, while low vitamin B12 [10] can contribute to fatigue, poor concentration and memory problems. A simple blood test can detect these deficiencies, and supplementation can make a meaningful difference to overall vitality.
Thyroid Function Test
The thyroid gland regulates metabolism, energy levels and mood. Both underactive and overactive thyroid conditions can cause vague symptoms such as weight changes, tiredness, palpitations or mood swings, which are often mistaken for normal ageing. A thyroid function test provides clarity and allows early treatment if needed.
How Often Should Seniors Get Screened?

Once the right tests have been identified, the next question is how often they should be repeated. The answer depends on the type of screening, existing health conditions and a senior’s overall risk profile. Generally, people over 50 years old are advised to undergo comprehensive health screening once a year. This provides a consistent overview of blood pressure, cholesterol, blood sugar and other routine checks that can change gradually with age.
Certain tests follow different schedules. For example, mammograms are typically recommended every two years, while bone density scans may only be needed every two to three years, depending on results and risk factors. Cancer screenings such as colonoscopy are carried out less frequently, but regular monitoring with the FIT kit may be advised on an annual basis.
Optional tests, such as vitamin and thyroid checks, may not need to be repeated regularly unless concerns arise. Doctors will usually advise whether follow-up is required, tailoring the frequency to each person.
The most effective approach is to work with a trusted healthcare provider to create a personalised screening plan. This ensures that seniors receive the right level of care without undergoing unnecessary tests, striking a balance between vigilance and practicality.
Cost, Subsidies and Accessibility in Singapore
One of the main concerns about health screening is cost. Fortunately, Singapore has made preventive care a national priority and several schemes are in place to ensure screenings remain affordable for seniors. These subsidies help alleviate financial concerns and encourage more people to take a proactive approach to their health.
| SCHEME | WHAT IT COVERS | HOW SENIORS BENEFIT |
| Healthier SG | Subsidised screening tests for conditions like diabetes, high blood pressure, high cholesterol and certain cancers. | Eligible Singaporeans aged 50 years and above can access screenings at highly reduced rates, sometimes paying only a few dollars. |
| Community Health Assist Scheme (CHAS) | Subsidies for medical and dental care at participating private clinics. | Seniors holding a CHAS card can enjoy lower costs for screening consultations and follow-up visits. |
| MediSave | Allows withdrawal of funds for specific screenings, such as colonoscopies, mammograms and other approved tests. | Seniors can use their MediSave savings to offset the cost of more advanced or one-off screening procedures. |
Screenings are widely available across Singapore, from polyclinics and restructured hospitals to private clinics and specialist centres. This ensures seniors can choose a convenient location that suits their preferences and comfort level. With subsidies and multiple care options in place, cost should never be a barrier to maintaining health.
Preparing for Your Health Screening
Knowing how to prepare for a health screening can make the process smoother and less stressful. Preparation varies depending on the type of tests, but a few simple steps can help seniors feel ready and confident.
For blood tests, fasting may be required for at least 8 to 10 hours beforehand, especially when checking cholesterol or blood sugar levels. It is important to continue taking prescribed medications unless advised otherwise by a doctor. Bringing along any past medical records, medication lists, or previous test results can also provide doctors with valuable context for comparison and informed decision-making.
On the day of the screening, wearing comfortable clothing and setting aside sufficient time for the appointment helps reduce anxiety. For seniors who may feel nervous, bringing a family member or caregiver along for support can make the experience more comfortable.
Most importantly, seniors should remember that screenings are not about finding faults but about gaining knowledge and reassurance. Understanding what to expect and being well-prepared allows the session to be more efficient, accurate and stress-free.
Taking Action After Screening Results

Completing a health screening is an important step, but what follows is just as crucial. Results are intended to guide the next course of action, whether that means maintaining current healthy habits or addressing newly discovered risks. To make the most of screening, seniors should take the following steps:
- Review results with a doctor – schedule a follow-up appointment to discuss findings. A doctor can explain what the results mean, whether additional tests are needed and how to manage any conditions detected.
- Follow recommended treatment or investigations – if abnormalities are found, act promptly. This may involve starting medication, adjusting existing treatment or undergoing further diagnostic procedures.
- Make lifestyle adjustments – adopt habits that support long-term health, such as balanced nutrition, regular physical activity, adequate sleep, reducing alcohol intake and avoiding smoking.
- Keep a record of results – maintain a personal health file with screening results over the years. Tracking changes helps doctors monitor trends and adjust care plans more effectively.
- Stay consistent with future screenings – use the results as motivation to keep up with regular check-ups. Screening is not a one-time effort but part of ongoing preventive care.
Screening results are not the end of the journey but the start of a proactive health plan. By taking timely action, seniors can preserve independence, reduce complications and enjoy a better quality of life.
Summary
Health screening after 50 years old is not simply about finding disease; it is about staying ahead of potential problems and ensuring a healthier, more independent future. With the right tests, timely action and supportive care, seniors in Singapore can look forward to living well as they age.
Key takeaways to remember:
- Screening saves lives – detecting conditions early leads to more effective treatment and better outcomes.
- Prevention is powerful – regular checks help prevent complications and maintain quality of life.
- Support is available – subsidies such as Healthier SG, CHAS and MediSave make health screening affordable and accessible.
- Action matters – following up with doctors and making lifestyle changes is just as important as the screening itself.
- Healthy ageing is achievable – with consistent care and proactive choices, seniors can enjoy many fulfilling years ahead.
Taking the first step towards health screening may feel daunting, but it is one of the most important investments seniors can make in themselves. If you or a loved one is over 50 years old, consult our doctors about the right tests and schedule a screening today. Remember: early action brings peace of mind, empowers healthier choices and paves the way for many more active and meaningful years ahead.
References
- Tenchov, R., Sasso, J. M., Wang, X., & Zhou, Q. A. (2024). Aging Hallmarks and Progression and Age-Related Diseases: A Landscape View of Research Advancement. ACS chemical neuroscience, 15(1), 1–30. https://doi.org/10.1021/acschemneuro.3c00531
- What is Healthier SG? (n.d.). In www.healthiersg.gov.sg. Retrieved September 1, 2025, from https://www.healthiersg.gov.sg/about/what-is-healthier-sg/
- Heart attacks remain on the rise in Singapore; experts say prudent to control risk factors. (n.d.). In CNA. Retrieved September 1, 2025, from https://www.channelnewsasia.com/singapore/heart-attacks-disease-rise-younger-people-risk-factors-5143436
- Lee, W. R. W. (2000). The changing demography of diabetes mellitus in Singapore. In Diabetes Research and Clinical Practice (Vol. 50, pp. S35–S39). Elsevier BV. https://doi.org/10.1016/s0168-8227(00)00184-4
- Rozhok, A. I., & DeGregori, J. (2016). The evolution of lifespan and age-dependent cancer risk. Trends in cancer, 2(10), 552–560. https://doi.org/10.1016/j.trecan.2016.09.004
- Osteoporosis. (2022). In National Institute on Aging. https://www.nia.nih.gov/health/osteoporosis/osteoporosis
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Public Health Approaches to Reduce Vision Impairment and Promote Eye Health (Eds.). (2016, September 15). Making eye health a population health imperative: Vision for tomorrow (Chapter 3: The Impact of Vision Loss). National Academies Press (US). Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK402367/
- Sharma, R. K., Chern, A., & Golub, J. S. (2021). Age-Related Hearing Loss and the Development of Cognitive Impairment and Late-Life Depression: A Scoping Overview. Seminars in hearing, 42(1), 10–25. https://doi.org/10.1055/s-0041-1725997
- Kaur J, Khare S, Sizar O, et al. Vitamin D Deficiency. [Updated 2025 Feb 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532266/
- Harvard Health Publishing Staff. (2013). Vitamin B12 deficiency can be sneaky and harmful. In Harvard Health. https://www.health.harvard.edu/blog/vitamin-b12-deficiency-can-be-sneaky-harmful-201301105780
- Memory Problems, Forgetfulness, and Aging. (2023). In National Institute on Aging. https://www.nia.nih.gov/health/memory-loss-and-forgetfulness/memory-problems-forgetfulness-and-aging

As a parent, you want to give your child the best possible start in life, and that includes protecting their long-term health. One important step is the human papillomavirus (HPV) vaccine, which protects against the virus. HPV is extremely common and is linked to several cancers and conditions that can affect both men and women.
The good news is that HPV-related diseases are largely preventable with vaccination. For many parents in Singapore, the question is not just whether the vaccine is necessary, but also when their teen should receive it, how safe it is, and what to expect.
This guide will walk you through everything you need to know about the HPV vaccine, based on current recommendations and clinical evidence.
What is HPV and Why is it a Concern?
HPV, or human papillomavirus, is one of the most prevalent viral infections worldwide. It is estimated that more than half [1] of sexually active people will be exposed to HPV at some point in their lives. The virus spreads primarily through skin-to-skin and sexual contact, and because it is so common, most people who contract HPV may not even realise it.
The body’s immune system often clears the infection naturally within a year or two. However, some HPV strains are more persistent [2]. When these high-risk types remain in the body, they can cause changes in cells that may develop into cancer years or even decades later.
The high-risk HPV strains are strongly associated with several cancers, including:
- Cervical cancer in women, where almost all cases [3] are linked to HPV infection
- Anal, penile, and throat cancers in both [4] men and women
- Oropharyngeal cancers [5] (back of the throat, tonsils, base of the tongue) are increasing [6] in incidence worldwide
Meanwhile, low-risk strains of HPV, although not cancer-causing, are responsible for genital warts [7], a common and distressing condition that can affect self-esteem and relationships.
In Singapore, cervical cancer continues to be a significant concern [8], ranking among the top 10 cancers in women. According to local statistics, hundreds of women are diagnosed every year, with many cases detected in their 30s to 50s. This is an age range when women are often balancing careers, families, and personal commitments.
What is important to remember is that HPV-related diseases are largely preventable. By vaccinating your teens before they are exposed to the virus, you are providing them with a powerful layer of protection against cancer and other HPV-related conditions later in life.
How Does the HPV Vaccine Work?

The HPV vaccine is designed to teach the body’s immune system how to recognise and fight HPV before an actual infection occurs. It contains virus-like particles (VLPs) that resemble the outer shell of the human papillomavirus but contain no genetic material. This means the vaccine cannot cause HPV infection.
Once the vaccine is given, the immune system responds by producing antibodies that remain in the body for years. If your teens are later exposed to HPV, these antibodies act like a protective shield, neutralising the virus before it can cause any damage.
This pre-emptive protection is why vaccination works best before HPV exposure, ideally during the teenage years.
Gardasil-4 vs Gardasil-9: What is the Difference?
Parents may come across two versions of the HPV vaccine: Gardasil-4 and Gardasil-9. It can be confusing to know which one is more suitable for their teens. Both vaccines are designed to protect against the most dangerous strains of HPV, but the difference lies in the breadth of coverage.
- Gardasil-4 was the earlier version and protects against four HPV types:
- HPV 16 and 18 – these are high-risk strains responsible for about 70% of cervical cancers [9] worldwide. They are also linked to other cancers, including anal, penile, and throat cancers.
- HPV 6 and 11 – these are low-risk strains that do not cause cancer but are responsible for about 90% of genital warts [10]. While not life-threatening, genital warts can be distressing, difficult to treat, and may recur.
- Gardasil-9 builds on this protection by covering the same four strains as Gardasil-4 plus five additional high-risk strains: 31, 33, 45, 52, and 58. These added strains are significant because they account for an additional 20% of cervical cancers globally [11]. By including them, Gardasil-9 protects against about 90% of all cervical cancers, as well as other HPV-related cancers in both men and women.
This broader coverage is why Gardasil-9 is now the standard vaccine in Singapore. It offers families greater reassurance that their teens are receiving more comprehensive protection available today.
At What Age Should My Teen Get the HPV Vaccine?
Timing is crucial for HPV vaccination. Both the World Health Organization (WHO) and the Ministry of Health (MOH) in Singapore recommend vaccination during adolescence, ideally before the onset of sexual activity.
Generally, the time frame is as follows:
- The optimal age is 9 to 14 years old, when the immune system produces a stronger and more effective response to the vaccine.
- Both girls and boys should receive the HPV vaccine. HPV does not only affect women. It can cause cancers of the throat, anus, and penis in men as well. Vaccinating boys also helps reduce HPV circulation in the community.
- For those who missed vaccination in early adolescence, a catch-up programme is available up to age 26 years old, ensuring young adults can still benefit from protection.
Is the HPV Vaccine Safe for Teenagers?

When it comes to any vaccine, safety is often the first question on a parent’s mind. The HPV vaccine has one of the most extensively studied safety records among modern vaccines. Since its introduction more than 15 years ago, over 500 million doses have been administered worldwide. Data from numerous large-scale studies, as well as continuous monitoring by global health authorities, show that the vaccine is both safe and effective.
Common, short-term side effects
Like many other routine vaccines, the HPV vaccine may cause mild and temporary side effects. These include:
- A low-grade fever
- Headache, tiredness, or mild muscle aches
- Soreness, redness, or swelling at the injection site
These reactions are usually short-lived, lasting a day or two, and indicate that the immune system is responding to the vaccine.
Rare, serious side effects
Serious side effects are extremely rare. Ongoing global safety monitoring has found no consistent evidence [12] linking the HPV vaccine to long-term complications. The vaccine’s safety record is comparable to other widely used childhood and adolescent vaccines.
Myths and misconceptions
Misinformation online has led some parents to worry about issues such as infertility, autoimmune conditions, or chronic illnesses. Extensive scientific research has confirmed that the HPV vaccine does not cause infertility or affect long-term health. Multiple studies conducted across different populations and age groups have consistently reached the same conclusion, which is that the HPV vaccine is safe.
Local reassurance in Singapore
In Singapore, all vaccines, including Gardasil 9, are strictly regulated by the Health Sciences Authority (HSA). The HSA continuously monitors vaccine safety and effectiveness, giving parents the added assurance that their teen is receiving a trusted and thoroughly vetted vaccine.
How Many Doses for HPV Are Needed and What’s the Schedule?
The number of doses required depends on your child’s age at the time of vaccination. This is because younger immune systems tend to respond more efficiently, meaning fewer doses are needed for lasting protection.
The timeline generally looks like:
- Ages 9 to 14 years – only 2 doses are needed. The second dose is given 6 to 12 months after the first.
- Ages 15 to 26 years – a 3-dose schedule is recommended. The doses are spaced at 0, 2, and 6 months.
If your teens miss a scheduled dose, there is no need to restart the entire course. Our doctor will adjust the timing to ensure the series is completed. What matters most is that your teens receive the full set of doses, as this ensures protection against HPV.
Is the HPV Vaccine Subsidised in Singapore?
The HPV vaccine is part of Singapore’s broader strategy to prevent cancer and protect population health. To make it more accessible for families, several subsidy schemes are in place:
- School-Based HPV Vaccination Programme – secondary girls are eligible to receive the HPV vaccine at no cost, administered directly in school as part of the national health initiative.
- CHAS and MediSave – Singapore Citizens can use CHAS subsidies and claim up to SGD500 yearly from MediSave per account to offset the cost of HPV vaccination at approved clinics. This makes vaccination more affordable for families of different income levels.
- Public and private clinics – HPV vaccination is widely available. While public clinics typically follow national subsidy schemes, private clinics may also offer packages for the full vaccination series.
What Should I Expect During My Teen’s HPV Vaccination Appointment?
For many parents and teens, knowing what to expect can help reduce any nervousness about vaccination. The process is simple, efficient, and usually completed within half an hour.
It entails:
- Pre-vaccination check – our doctor will review your teen’s health history, allergies, and suitability for the vaccine. This step ensures that your child is medically fit for vaccination.
- Injection – the vaccine is given as a quick injection in the upper arm. The procedure is similar to other routine vaccinations and is usually well-tolerated.
- Observation period – after the injection, your teen will remain in the clinic for about 15 minutes. This is standard practice to ensure there are no immediate side effects.
- Post-care – mild arm soreness or a temporary fever may occur, but typically resolves quickly. Most teens can return to school, sports, or their usual activities straight after the appointment.
Our clinic will also schedule reminders for the next dose, helping your teen stay on track to complete the full vaccination series.
Give Your Teen a Head Start on Health
The HPV vaccine is a safe and effective tool in preventing HPV-related cancers and diseases. By choosing to vaccinate your teens, you are investing in their long-term health and protecting them from conditions that may only surface decades later.
At Ardennes, we understand that parents want clear answers and reliable guidance when it comes to their child’s health. Our doctors are here to provide professional advice, address your concerns, and ensure your teens receive the best care.
Book an HPV vaccine appointment with Ardennes today and give your teen the protection they deserve.
References
- Ault K. A. (2006). Epidemiology and natural history of human papillomavirus infections in the female genital tract. Infectious diseases in obstetrics and gynecology, 2006 Suppl, 40470. https://doi.org/10.1155/IDOG/2006/40470
- So, K. A., Lee, I. H., Lee, K. H., Hong, S. R., Kim, Y. J., Seo, H. H., & Kim, T. J. (2019). Human papillomavirus genotype-specific risk in cervical carcinogenesis. Journal of gynecologic oncology, 30(4), e52. https://doi.org/10.3802/jgo.2019.30.e52
- Cervical Cancer Causes, Risk Factors, and Prevention – NCI. (2022). In www.cancer.gov. https://www.cancer.gov/types/cervical/causes-risk-prevention
- Baba, S. K., Alblooshi, S. S. E., Yaqoob, R., Behl, S., Al Saleem, M., Rakha, E. A., Malik, F., Singh, M., Macha, M. A., Akhtar, M. K., Houry, W. A., Bhat, A. A., Al Menhali, A., Zheng, Z. M., & Mirza, S. (2025). Human papilloma virus (HPV) mediated cancers: an insightful update. Journal of translational medicine, 23(1), 483. https://doi.org/10.1186/s12967-025-06470-x
- Sabatini, M. E., & Chiocca, S. (2020). Human papillomavirus as a driver of head and neck cancers. British journal of cancer, 122(3), 306–314. https://doi.org/10.1038/s41416-019-0602-7
- Hussein, A. A., Helder, M. N., de Visscher, J. G., Leemans, C. R., Braakhuis, B. J., de Vet, H. C., & Forouzanfar, T. (2017). Global incidence of oral and oropharynx cancer in patients younger than 45 years versus older patients: A systematic review. In European Journal of Cancer (Vol. 82, pp. 115–127). Elsevier BV. https://doi.org/10.1016/j.ejca.2017.05.026
- Bhatia, N., Lynde, C., Vender, R., & Bourcier, M. (2013). Understanding genital warts: epidemiology, pathogenesis, and burden of disease of human papillomavirus. Journal of cutaneous medicine and surgery, 17 Suppl 2, S47–S54
- Chan, Y.M., Ismail, M.Z.H. & Khaw, WF. Factors influencing the prevalence of cervical cancer screening in Malaysia: a nationwide survey. BMC Women’s Health 23, 389 (2023). https://doi.org/10.1186/s12905-023-02553-3
- Works Cited Ramakrishnan, S., Partricia, S., & Mathan, G. (2015). Overview of high-risk HPV’s 16 and 18 infected cervical cancer: Pathogenesis to prevention. In Biomedicine & Pharmacotherapy (Vol. 70, pp. 103–110). Elsevier BV. https://doi.org/10.1016/j.biopha.2014.12.041
- Genital Warts (Condylomata Acuminata): Background, Pathophysiology, Etiology. (2025). https://emedicine.medscape.com/article/763014-overview?form=fpf
- Human Papillomavirus (HPV) Vaccines – NCI. (2024). In www.cancer.gov. https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-vaccine-fact-sheet
- Parent Concerns About HPV Vaccine Safety Increasing – NCI. (2021). In www.cancer.gov. https://www.cancer.gov/news-events/cancer-currents-blog/2021/hpv-vaccine-parents-safety-concerns
- Schmuhl, N. B., Mooney, K. E., Zhang, X., Cooney, L. G., Conway, J. H., & LoConte, N. K. (2020). No association between HPV vaccination and infertility in U.S. females 18-33 years old. Vaccine, 38(24), 4038–4043. https://doi.org/10.1016/j.vaccine.2020.03.035

Sexual health is a vital part of overall well-being, yet for many, the topic of sexually transmitted diseases (STDs) remains surrounded by stigma, silence and misinformation. This often leads to delays in seeking medical help, increasing the risk of complications and further transmission.
In Singapore, the issue is more common than many realise. In 2024, there were 151 new HIV cases [1] — the lowest annual total since 1998 — yet over half were diagnosed at a late stage, pointing to a worrying trend of delayed detection. Among notifiable sexually transmitted infections [2] (STIs), chlamydia remains the most commonly reported [3], followed by syphilis and gonorrhoea.
These numbers serve as a reminder: STDs are more widespread and often overlooked than we think. The first step to protecting your health is being informed. In this blog, we break down the facts about common STDs: how they spread, the symptoms to look out for, when to get tested, and the treatment options available.
What are Sexually Transmitted Diseases (STDs)?
STDs, also referred to as STIs, are infections that primarily spread through sexual contact. This includes vaginal, anal or oral sex. In some cases, it can be spread through skin-to-skin contact.
While “STD,” and “STI” are often used interchangeably, the term STI is more accurate in many cases. This is because not all infections cause disease or symptoms. In fact, someone may have an infection and pass it on without even knowing.
How do Sexually Transmitted Diseases spread?
Bacteria, viruses or parasites are the known causes of STDs. As such, they are most transmitted through:
- Unprotected vaginal, anal or oral sex
- Genital-to-genital contact
- Sharing needles or syringes
- During childbirth (mother to baby)
- In rare cases, through blood transfusions or organ transplants
It is important to remember that STDs cannot spread through casual contact such as hugging, sharing food or using the same toilet.
What are the common Sexually Transmitted Diseases?
Although STDs are common in Singapore, social stigma combined with a lack of awareness often results in many cases going undetected. This is especially common in the early stages, where the disease may not cause noticeable symptoms.
Knowing the common types, how they are caused and what to look out for can help you seek timely testing and treatment. Some of the common STDs are:
| STD | CAUSE | WHAT IT IS | KEY CHARACTERISTICS / APPEARANCE |
| Chlamydia | Bacteria (Chlamydia trachomatis) | A common bacterial infection affecting the genitals, rectum or throat. | Often silent. It may cause abnormal discharge, pain during urination or pelvic pain. |
| Gonorrhoea | Bacteria (Neisseria gonorrhoeae) | A bacterial infection that can affect the genitals, rectum and throat. | Yellow or green discharge, painful urination or sore throat (if oral). |
| Syphilis | Bacteria (Treponema pallidum) | A bacterial infection that progresses in stages, from sores to serious organ damage if untreated. | Painless sore, followed by rashes, fever and in late stages, neurological or heart issues. |
| Genital Herpes | Virus (Herpes Simplex Virus – HSV-1 or HSV-2) | A viral infection that causes recurrent sores on the genital or oral area. | Painful blisters or ulcers on or around the genitals, anus or mouth. It may recur after treatment. |
| Human Papillomavirus (HPV) | Virus | A group of viruses, some of which cause genital warts or lead to cervical and other cancers. | Genital warts (small bumps, often clustered). However, most strains are asymptomatic. |
| HIV | Virus (Human Immunodeficiency Virus) | A virus that weakens the immune system and can lead to AIDS if untreated. | Flu-like symptoms early on. However, later stages involve fatigue, weight loss and recurrent infections. |
| Hepatitis B | Virus | A viral infection affecting the liver, which can be transmitted sexually or through blood. | May be silent. Some experience fatigue, jaundice or liver inflammation. |
| Trichomoniasis | Parasite (Trichomonas vaginalis) | A parasitic infection commonly affects the genital tract. | Foul-smelling vaginal discharge, itching and irritation. But it is often asymptomatic in men. |
What are the signs and symptoms of Sexually Transmitted Diseases?
Many STDs are asymptomatic, especially in the early stages. This is why regular screening is important if you are sexually active. When symptoms appear, they may include:
- Flu-like symptoms (fever, fatigue, swollen glands)
- Genital sores, blisters or warts
- Itching, redness or swelling in the genital area
- Lower abdominal or pelvic pain
- Pain during intercourse
- Pain or burning during urination
- Rectal pain, discharge or bleeding
- Unusual vaginal or penile discharge
What happens if Sexually Transmitted Diseases are left untreated?
Whether symptoms are mild or asymptomatic, it is crucial not to ignore the possibility of an STD. Many infections can silently progress and cause serious long-term health consequences.
This includes:
- Chronic pain – pelvic pain [4], testicular discomfort and pain during intercourse are possible long-term effects of untreated infections. These symptoms can persist even after the infection is cleared. It may also affect daily functioning and quality of life.
- Infertility – infections like chlamydia and gonorrhoea can spread to the reproductive organs, causing pelvic inflammatory disease (PID) in women and epididymitis in men. These conditions can result in permanent damage [5], making it difficult or impossible to conceive naturally.
- Pregnancy complications – STDs during pregnancy [6] can lead to miscarriage, preterm birth or low birth weight. Some infections, like syphilis or herpes, can also be passed from mother to baby during childbirth. This may potentially cause serious neonatal infections or congenital abnormalities.
- Organ damage and systemic illness – some infections can progress to affect the heart, liver, brain and nervous system. This is especially risky with syphilis [7], hepatitis B/C [8] and HIV [9].
The good news is that many STDs can be easily treated if caught early. That is why seeking timely medical attention is crucial, as it can improve the outcomes of the treatment while safeguarding your sexual health.
How are Sexually Transmitted Diseases diagnosed?

Doctors will initially begin the diagnostic process with a medical evaluation. During this stage, doctors may ask questions such as:
- The symptoms you are experiencing
- How long have you experienced these symptoms
- Risk factors, such as lifestyle
- Your medical history
- Your sexual history, which includes how many partners you have had
These answers will then help doctors determine the combination of methods tailored to the type of infection. It may include:
- Blood tests – detect antibodies, antigens or DNA/RNA for infections like HIV, syphilis, herpes and hepatitis B/C.
- Urine tests – use Nucleic Acid Amplification Tests (NAATs) to identify bacterial DNA for chlamydia or gonorrhoea.
- Swab tests – PCR-based swabs for genital areas, throat, rectum or sores. It is often used for chlamydia, gonorrhoea, herpes or HIV.
- Multiplex PCR panels – they offer comprehensive screening for multiple infections from a single sample.
When should you get tested for STDs?
Early detection saves lives, prevents complications and most importantly, stops transmission. As such, here is when you should consider getting tested for an STD:
- After a possible exposure – if you have had unprotected sex, engaged in a new or casual partner or suspect your partner may be infected, then it’s recommended to get yourself tested. Testing should follow the recommended windows as below:
- Retesting for chlamydia 1 to 3 weeks after the initial test (even if the first result came back negative).
- Retesting for syphilis 3 to 6 weeks after the initial test (even with a negative result from the first test).
- If you have symptoms – even if you are experiencing mild symptoms like burning sensation while urinating, unusual discharge, sores or rashes, this warrants immediate testing.
- For routine checks – Singapore’s National HIV Testing Recommendations advise that every adult (age 21 years and older) should get tested for HIV at least once in their lifetime. Meanwhile, higher risk individuals are encouraged to get tested every 3 to 6 months.
- When a partner tests positive – if your partner is diagnosed with an STD, do get tested immediately. Even in the absence of symptoms, STDs can still spread easily and silently.
How are Sexually Transmitted Diseases treated?

Being diagnosed with an STD can feel overwhelming. However, you are not alone and help is available.
Most STDs are treatable and many can be completely cured with the right medical care. For those that are not curable, effective treatments can help you live well, manage symptoms and prevent transmission to others. Starting treatment early not only protects your health, but also your future relationships and well-being.
Depending on the cause, STDs are treated through:
Bacterial STDs (curable)
- Chlamydia – typically treated with doxycycline for 7 days. Pregnant ladies who are diagnosed with this disease are treated with azithromycin.
- Gonorrhoea – often treated with antibiotics such as ceftriaxone, combined with azithromycin.
- Syphilis – penicillin is the standard treatment, with alternatives available for those allergic.
Viral STDs (manageable, but not curable)
- Genital herpes – antivirals like acyclovir reduce outbreaks and transmission risk.
- HIV – requires lifelong antiretroviral therapy (ART). Over 90% of Singaporean residents on ART achieve an undetectable viral load, virtually eliminating transmission risk.
- HPV – no cure, but vaccination helps. Additionally, HPV-linked cancers are monitored and managed.
- Hepatitis B/C – chronic cases are monitored and treated to manage symptoms and improve quality of life.
Why is follow-up care important?
Treatment is only one part of the journey towards better sexual health. Proper follow-up care plays a crucial role in ensuring that infections are fully cleared, chronic conditions are well managed and partners are protected from reinfection.
Whether your diagnosis was bacterial or viral, taking the right steps after treatment can safeguard your long-term health and support the well-being of those around you.
A comprehensive follow-up care involves:
| STEPS | WHAT IT ENTAILS |
| Retesting to Confirm a Cure (for Bacterial STDs) | Even if symptoms have resolved, it is important to retest after treatment. It is typically done 2 to 4 weeks later, depending on the type of infection and your doctor’s advice. This is especially important for:ChlamydiaGonorrhoeaSyphilis Retesting ensures the infection has fully cleared and helps detect possible reinfection, which is not uncommon. For example, some studies show up to 20% of people treated for chlamydia may get reinfected within a few months, often unknowingly. |
| Ongoing Monitoring (for Chronic Viral STDs) | For viral infections such as HIV, herpes, HPV and hepatitis B/C, follow-up care is ongoing and vital. These infections may not be curable, but they can be effectively managed with regular medical support. Monitoring typically includes: HIV – regular blood tests to check viral load and CD4 counts. Adhering to ART can reduce viral load to undetectable levels, which means zero risk of transmission to others through sex.Hepatitis B/C – periodic liver function tests and ultrasounds may be needed to check for signs of liver damage, cirrhosis or cancer.Herpes and HPV – monitoring focuses on symptom control and regular screening to catch potential complications early. |
| Partner Notification and Support | If you have been diagnosed with an STD, it is crucial to let your sexual partner(s) know, even if you are no longer in contact. This may feel uncomfortable, but open communication helps stop the cycle of reinfection and protects others from unknowingly spreading an infection. You do not have to do it alone. In Singapore, many clinics and local non-governmental organisations (NGOs) offer:Anonymous partner notification servicesCounselling and educational resourcesSupport groups or helplines |
Final Thoughts
STDs are more common than many people think. What is even more unfortunate is that it often goes unnoticed until complications arise. But the truth is: most STDs are treatable and many are completely curable, especially when caught early. Even chronic infections like HIV or herpes can be managed effectively with modern treatment, allowing individuals to lead healthy, fulfilling lives.
Unfortunately, many delay seeking help due to fear, shame or misconceptions. However, it’s important to remember that there is no shame in getting tested. In fact, prioritising your health is an act of self-respect and it protects those around you too. Like any other medical issue, STDs deserve to be handled with dignity, compassion and science-based care.
If you are experiencing potential symptoms of an STD, schedule a consultation with us today for a detailed diagnosis and treatment plan.
References
- Sexual Health. (2025). In Default. Default. https://www.nus.edu.sg/uhc/health-promotion/sexual-health
- Sexually Transmitted Infections. (n.d.). In www.healthhub.sg. Retrieved June 30, 2025, from https://www.healthhub.sg/programmes/sexually-transmitted-infections
- Chlamydia. (n.d.). In Communicable Diseases Agency. Retrieved June 30, 2025, from https://www.cda.gov.sg/professionals/diseases/chlamydia
- Jennings LK, Krywko DM. Pelvic Inflammatory Disease. [Updated 2023 Mar 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499959/
- Tsevat, D. G., Wiesenfeld, H. C., Parks, C., & Peipert, J. F. (2017). Sexually transmitted diseases and infertility. American journal of obstetrics and gynecology, 216(1), 1–9. https://doi.org/10.1016/j.ajog.2016.08.008
- Kumar, M., Saadaoui, M., & Al Khodor, S. (2022). Infections and Pregnancy: Effects on Maternal and Child Health. Frontiers in cellular and infection microbiology, 12, 873253. https://doi.org/10.3389/fcimb.2022.873253
- Tudor ME, Al Aboud AM, Leslie SW, et al. Syphilis. [Updated 2024 Aug 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534780/
- Hepatitis B and the liver: What to know. (2024). In www.medicalnewstoday.com. https://www.medicalnewstoday.com/articles/does-hepatitis-b-attack-the-liver
- Neurological Complications of HIV. (n.d.). Retrieved July 1, 2025, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/hiv-and-aids/neurological-complications-of-hiv

When was the last time you thought about your cervical health?
For many women, it rarely crosses the mind, especially when there are no symptoms. Life gets busy, appointments get delayed, and screening often slips to the bottom of the list. Yet cervical cancer doesn’t wait. It develops quietly, often without warning, and by the time symptoms appear, it may already be advanced.
In Singapore, cervical cancer remains one of the top ten cancers affecting women [1]. But it is also one of the most preventable. The key lies in early detection — and that begins with a simple, routine test: the Pap smear.
Despite widespread availability and decades of medical evidence supporting its effectiveness, screening rates in Singapore are still not where they should be. Some women are unsure when to start or how often to go. Others feel anxious or embarrassed, or don’t know what the procedure involves. This lack of awareness and confidence can lead to delays in diagnosis and missed opportunities for early treatment.
This guide is here to change that. Whether you are 25 and preparing for your first test, or 45 and unsure if you are overdue, this article offers a clear and practical overview of Pap smears in Singapore. We will explain what the test is, why it matters, who needs it, how often it’s recommended, and where you can get it done.
Understanding Pap Smears
Cervical cancer screening can feel unfamiliar or even intimidating, especially if it’s your first time. But understanding what a Pap smear is and how it works is the first step toward making confident, informed choices about your health. Here is what the test involves and how it compares with another common screening method: the HPV test.
What is a Pap smear?
A Pap smear is a screening test used to detect abnormal changes in the cells of the cervix [2]. These changes, if left untreated, can develop into cervical cancer over time. During the test, a healthcare provider uses a small brush or spatula to gently collect cells from the cervix. The sample is then sent to a laboratory for examination under a microscope.
The main goal of a Pap smear is to find early warning signs — cellular changes that aren’t yet cancer, but could become cancer if not managed. Detecting these abnormalities early allows for simple and effective treatment, long before cancer has a chance to develop.
The procedure is quick, typically taking less than five minutes. It may feel slightly uncomfortable, but it should not be painful, and no recovery time is needed afterward.

Pap Smear vs HPV Test — What’s the Difference?
While both the Pap smear and HPV test are used in cervical cancer screening, they test for different things and are recommended at different stages of life. Understanding the distinction helps clarify which test you need and why.
| Aspect | Pap Smear | HPV Test |
| What it checks for | Abnormal or precancerous cells on the cervix | Presence of high-risk HPV strains that can cause cervical cancer |
| Purpose | Detects early cellular changes | Detects the virus that causes those cellular changes |
| Recommended age group | Women aged 25–29 | Women aged 30–69 |
| Screening interval | Every 3 years | Every 5 years |
| Used for | Early detection of abnormal cells | Identifying high-risk HPV before cell changes occur |
| Can it be done together? | Sometimes recommended as a co-test depending on history | Yes, often combined with Pap smear in women over 30 |
Both tests play a role in safeguarding cervical health. Your doctor will recommend the appropriate test based on your age, screening history, and overall risk profile.
Cervical Cancer in Singapore
Cervical cancer remains a serious yet largely preventable health concern for women. The availability of screening and vaccination has significantly improved early detection, but the burden of the disease persists — particularly when regular screening is delayed or skipped. In Singapore, the patterns of diagnosis and the factors that increase risk highlight the ongoing need for awareness and timely intervention.
Prevalence and Statistics
According to the Singapore Cancer Registry, cervical cancer ranks among the top ten most common cancers in women [3]. Each year, around 200 women are diagnosed, and approximately 70 lose their lives to the disease [4]. Although the incidence has declined over the decades—thanks to improved access to Pap smears and the introduction of HPV vaccination—the rates are still concerning, particularly among women who do not undergo regular screening.
Data shows that the risk of cervical cancer increases with age, and many of the cases diagnosed are in women who have either never been screened or have not had a Pap smear in the last five years. This underlines the importance of consistent follow-up, especially in women aged 30 and above.
Risk factors
Several well-established factors can increase a woman’s risk of developing cervical cancer. Understanding these risks is key to recognising the importance of regular screening:
- Persistent HPV infection — the most significant risk factor. High-risk strains of the human papillomavirus (especially HPV 16 and 18) are responsible for the majority of cervical cancer cases [5].
- Smoking — chemicals in tobacco can damage cervical cells, making them more susceptible to HPV-related changes [6].
- Early sexual activity or multiple sexual partners — these factors increase the likelihood of HPV exposure.
- Weakened immune system — conditions like HIV [7] or long-term use of immunosuppressive medication can reduce the body’s ability to fight HPV infections.
- Lack of regular screening — women who have never had a Pap smear or have infrequent screenings face a significantly higher risk of late-stage diagnosis.
- Long-term use of oral contraceptives — some studies suggest a slightly increased risk after five or more years of continuous use [8].
While not all risk factors can be controlled, regular screening and HPV vaccination remain the most effective tools for prevention and early detection of cervical cancer.
National Guidelines for Cervical Cancer Screening
Cervical cancer screening is not a one-size-fits-all process. In Singapore, national guidelines are tailored to maximise the benefits of screening while minimising unnecessary procedures. The Ministry of Health has established age-based recommendations to ensure that women receive the most suitable test at the appropriate time.
Understanding these guidelines can help you stay on track with your screenings, avoid confusion about when to start or stop, and ensure you’re receiving the most relevant care for your age and risk profile. Here are the recommended screening ages and intervals [9].
Women aged 25 to 29
Cervical screening is recommended for women based on their age, and sexual history:
- Women aged 25 years old, and above who have ever had sexual intercourse should begin regular cervical cancer screening at 25 years old.
- Women who have never had sexual intercourse do not require cervical screening. However, if they experience symptoms such as abnormal vaginal bleeding, then they should consult a doctor
Additionally, this group of women is encouraged to undergo a routine pap smear every 3 years. At this age, Pap smears are preferred over HPV tests because younger women are more likely to clear HPV infections naturally, and over-testing may lead to unnecessary interventions.
Women aged 30 to 69
Women between the ages of 30 to 69 should undergo an HPV test every 5 years if the result is negative. The HPV test is more accurate in detecting high-risk HPV strains, and is now the primary screening tool for women in this age group. It can identify risk earlier, even before any visible cellular changes occur.
Women in both age groups should ensure that their screenings are up to date, even if they have no symptoms and feel well. Regular screening is preventive, not reactive—it’s meant to catch changes before they cause harm.
Women who have had HPV Vaccination
Women who have received the HPV vaccine should continue to follow the same screening schedule as those who are unvaccinated.
Immunocompromised women
Women with weakened immune systems, including those on long-term immunosuppressive therapy, may require more frequent screening. These cases should be assessed, and managed individually by a gynaecologist.
Special Considerations
Women over 69
Women in this age group may stop screening if they have had two consecutive negative HPV tests in the last 10 years, with the most recent test within the past 5 years. Those with a history of abnormal results may still require continued monitoring.
Meanwhile, women with a history of treatment for CIN 2, CIN 3, or adenocarcinoma in situ (AIS) should continue routine screening for at least 20 years, even if this extends beyond the age of 69 years old.
Women who have had a hysterectomy
The need for continued cervical screening depends on the type of hysterectomy, and the woman’s medical history. This includes:
Total hysterectomy for benign conditions
Further cervical cancer screening is only needed if:
- The woman has a history of normal cervical cytology.
- Histopathology confirms the cervix was benign with no precancerous or cancerous changes.
Subtotal (partial) hysterectomy
Cervical screening should continue according to the national screening guidelines, as the cervix remains in place.
Hysterectomy where cervical histology is unknown
For women in this group, a baseline vaginal vault smear is recommended. However, if the result is normal, then no further screening is necessary.
Histology of cervical intraepithelial neoplasia (CIN)
If the excision margins were involved or not adequately assessed, follow-up should be guided by a gyneacologist. In general, vault smears should be taken at least annually.
Additionally, if CIN (Cin 1/2/3) was completely excised at the time of hysterectomy:
- Vault smears should be done annually for 5 years.
- Then, every 2 years for an additional period as advised by the clinician.
Preparing for a Pap Smear
Feeling uncertain before a Pap smear is completely normal, especially if it’s your first time. Knowing how to prepare can help ease any anxiety, ensure the most accurate results, and make the experience as smooth as possible.
Optimal Timing
The best time to schedule a Pap smear is about 10 to 20 days after the first day of your periods, when you are not menstruating. While it is still possible to perform the test during light bleeding, heavy menstrual flow may interfere with the accuracy of the cell sample. If your cycle is unpredictable, let the clinic know in advance so they can advise on the best timing.
Before the Test: What to Avoid
To ensure the best quality sample, it’s recommended to avoid the following 24 to 48 hours before your appointment:
- Sexual intercourse — seminal fluid and friction can temporarily affect cervical cells and obscure results.
- Douching or vaginal washes —these can disrupt the natural environment of the cervix and wash away or alter the cells that need to be examined.
- Tampons, vaginal creams, suppositories, or lubricants — these products can interfere with sample collection and analysis.
If you are unsure whether your recent activities could affect your results, speak with your healthcare provider before the test. It’s also perfectly acceptable to ask questions during the appointment or request a female provider if that makes you more comfortable.
Being well-prepared not only helps your doctor perform the test efficiently but also increases the likelihood of a clear and conclusive result — avoiding the need for a repeat test.
The Pap Smear Procedure
Understanding what happens during a Pap smear can help reduce uncertainty and make the experience more manageable. The test itself is quick and usually takes only a few minutes. While it may feel unfamiliar or slightly uncomfortable, it is not typically painful — and your doctor will guide you through each step.
What to Expect During the Test
You will begin by lying on an examination table, typically with your knees bent and feet placed in stirrups. A device called a speculum is gently inserted into the vagina to hold it open, allowing the doctor to clearly view the cervix.
Using a small, soft brush or spatula, the doctor will collect a sample of cells from the surface of your cervix. This may cause a slight scraping sensation or mild pressure, but it usually lasts only a few seconds. Once the sample is collected, the speculum is removed and the procedure is complete.
The entire process takes less than five minutes.
Is It Painful?
Most women describe the test as mildly uncomfortable rather than painful. Some may feel pressure or cramping similar to menstrual discomfort, especially if it’s their first time or if they are feeling tense. Taking slow, deep breaths and trying to stay relaxed can help ease any discomfort during the exam.
If you experience significant pain at any point, let your doctor know immediately, as it could indicate an underlying issue that may need further attention.
Being informed and knowing what to expect can make the experience much less stressful. If you have concerns or specific preferences — such as having a female doctor or being talked through the process in advance — don’t hesitate to request this when making your appointment.
Interpreting Pap Smear Results and What Happens Next
Once your Pap smear is complete, the collected sample is sent to a laboratory for analysis. Results are usually available within one to two weeks and will be shared with you by your doctor.
Pap smear results typically fall into one of three categories:
- Normal (negative) — this means no abnormal cells were found, and you can continue routine screening as advised based on your age.
- Abnormal — this indicates that some changes were detected in the cervical cells. It does not mean you have cancer, but further testing may be needed to determine the cause and whether treatment is necessary.
- Unsatisfactory — in some cases, the sample may not contain enough cells or may be obscured by blood or mucus. Your doctor may recommend repeating the test to ensure a clear reading.
If your result is abnormal, the next steps depend on the type and severity of the changes. Your doctor may recommend:
- A repeat Pap smear after a short interval
- An HPV test to check for high-risk viral strains
- A colposcopy, a procedure that allows the cervix to be examined more closely under magnification
- A biopsy (if further investigation is needed)
Timely follow-up is essential, even if you feel well. Many cervical cell changes cause no symptoms but can progress silently over time.
Cervical Cancer Screening in Singapore
Cost and convenience should never stand in the way of essential healthcare. While many women assume that cervical cancer screening is expensive or hard to access, the reality is quite the opposite — Pap smears and HPV tests are widely available across Singapore, often at highly subsidised rates.
For those seeking more personalised care, many private women’s clinics and GP practices offer Pap smears as part of health screening packages. At Ardennes Health, we provide discreet, comfortable, and professionally guided Pap smear screening in a calm, patient-centred setting. Whether you are coming in for your first test or a routine follow-up, our team is here to ensure you feel informed, supported, and cared for at every step.
With accessible options across both public and private sectors, there’s no reason to postpone your screening. What matters most is staying on schedule — because early detection saves lives.
Taking Charge of Your Cervical Health
Cervical cancer is one of the few cancers that can be prevented through early detection and timely treatment — and the Pap smear remains one of the most effective tools in achieving that. Yet, many women continue to miss out on screening due to uncertainty, discomfort, or the misconception that it’s unnecessary in the absence of symptoms.
Pap smear is a quick, safe, and reliable test that can detect changes in cervical cells long before they pose a serious threat. When combined with regular HPV testing and follow-up care, it offers women a powerful layer of protection against a disease that often develops without warning.
If you are due for a Pap smear or simply unsure where to begin, schedule a consultation with us for confidential, professional care tailored to your needs.
References
- Cervical cancer. Retrieved May 6, 2025, from https://www.singaporecancersociety.org.sg/learn-about-cancer/types-of-cancer/cervical-cancer.html
- What is a pap test? Cleveland Clinic. Retrieved May 6, 2025, from https://my.clevelandclinic.org/health/diagnostics/4267-pap-smear
- Singapore cancer society. Retrieved May 6, 2025, from https://singaporecancersociety.org.sg/index.php
- Cervical Cancer – What It Is. SingHealth. Retrieved May 6, 2025, from https://www.singhealth.com.sg/patient-care/conditions-treatments/cervical-cancer
- Okunade, K. S. (2020). Human papillomavirus and cervical cancer. Journal of Obstetrics and Gynaecology: The Journal of the Institute of Obstetrics and Gynaecology, 40(5), 602–608. https://doi.org/10.1080/01443615.2019.1634030
- Smoking and cervical cancer. Australian Government Department of Health and Aged Care. Retrieved May 6, 2025, from https://www.health.gov.au/our-work/tobaccofacts/smoking-and-cervical-cancer#:~:text=Chemicals%20from%20smoke%20change%20your,cells%20of%20women%20who%20smoke.
- Hewavisenti, R. V., Arena, J., Ahlenstiel, C. L., & Sasson, S. C. (2023). Human papillomavirus in the setting of immunodeficiency: Pathogenesis and the emergence of next-generation therapies to reduce the high associated cancer risk. Frontiers in Immunology, 14, 1112513. https://doi.org/10.3389/fimmu.2023.1112513
- Oral contraceptives (Birth control pills) and cancer risk—Nci. (2018, March 1). [cgvArticle]. https://www.cancer.gov/about-cancer/causes-prevention/risk/hormones/oral-contraceptives-fact-sheet
- Why annual pap smears are history – but routine ob-gyn visits are not. (n.d.). Retrieved May 6, 2025, from https://www.acog.org/womens-health/experts-and-stories/the-latest/why-annual-pap-smears-are-history-but-routine-ob-gyn-visits-are-not
- Enhanced screen for life(Sfl). Ministry of Health. Retrieved May 6, 2025, from https://www.moh.gov.sg/managing-expenses/schemes-and-subsidies/enhanced-screen-for-life/

Influenza, more commonly known as the flu, is a contagious respiratory illness caused by influenza viruses. In Singapore, the flu is fairly common, given the hot and humid weather all-year-round, creating a conducive environment for viruses to survive and circulate easily.
Flu vaccinations remain the most effective way to prevent influenza and its complications. It not only reduces the likelihood of falling ill but also limits the severity of symptoms if infection occurs. Moreover, getting vaccinated helps reduce the spread of the virus in the community as it protects those who are unable to receive the vaccine, such as very young infants or individuals with specific medical conditions. In this article, we’ll look into flu vaccinations in Singapore, who needs them, and why.
Understanding the Flu: Spread and Symptoms
Influenza is an acute viral infection caused by influenza viruses, which primarily affect the respiratory system. There are four main types of influenza viruses, A, B, C, and D, but only types A and B are responsible for seasonal flu outbreaks in humans [4]. These viruses are highly infectious and have the ability to mutate rapidly, resulting in new strains that can vary from year to year.
Influenza spreads mainly through droplets expelled when an infected person coughs, sneezes, or talks. These droplets can land in the mouths or noses of nearby individuals or be inhaled into the lungs. The virus can also spread through contact with contaminated surfaces, such as door handles or shared devices, followed by touching the face. Because it can be transmitted before symptoms appear and up to a week after falling ill, influenza is particularly difficult to contain without proactive measures like vaccination and good hygiene practices.
Potential complications of influenza include:
- Pneumonia — a serious lung infection that can be life-threatening, especially in the elderly and those with chronic illnesses.
- Sinus and ear infections — particularly in children.
- Exacerbation of chronic conditions — such as asthma, diabetes, and heart disease.
- Hospitalisation or death — in severe cases, particularly among vulnerable populations.

Why is the flu so common in Singapore?
The flu is relatively common in Singapore for the following reasons:
- Tropical climate — Because of Singapore’s constant warm and humid climate, influenza viruses can circulate all-year-round.
- High population density — Singapore is a densely populated urban society, which increases chances of person-to-person transmission.
- International travel hub — The country is well-known for being an international travel hub, increasing risk of imported flu strains.
- Enclosed environments — Enclosed, air-conditioned spaces are common in Singapore, and are conducive spaces for virus survival and transmission.
Who Should Consider a Flu Vaccine?
Influenza vaccination is recommended for everyone aged 6 months and older, with rare exceptions. The Ministry of Health (MOH) in Singapore [5], along with global health authorities such as the World Health Organization (WHO) [6], advises annual flu vaccination as a key preventive measure. This is because influenza viruses evolve constantly, and the vaccine is updated regularly to offer protection against the most common circulating strains.
While the general population can benefit from vaccination, certain groups face a significantly higher risk of developing serious complications from the flu. For these individuals, the flu vaccine is not only a preventive measure, it can be life-saving.
Elderly Individuals (65 years and Above)
Older adults are more vulnerable to severe flu-related illnesses [7]. With age, the immune system weakens, which minimises the body’s ability to fight infections effectively. Influenza in the elderly is more likely to lead to hospitalisation, pneumonia, and, in some cases, death. Annual vaccination offers critical protection by reducing the severity of illness and the risk of complications.
Young Children (6 months to Under 5 Years)
Young children, particularly those under five years of age, have less developed immune systems, which makes them more susceptible to influenza and its complications, including febrile seizures and respiratory infections [8]. The flu vaccine helps to strengthen their immunity and reduce transmission in childcare settings and homes.
Pregnant Women
Pregnant women are more prone to severe flu symptoms and complications, especially in the later stages of pregnancy [9]. Importantly, the flu vaccine also provides protection to the unborn child, with antibodies passed from mother to baby. Vaccination is safe during any trimester and is strongly recommended as part of routine maternal care.
Individuals with Chronic Medical Conditions
People living with chronic conditions such as diabetes, asthma, chronic lung disease, heart disease, or compromised immune systems are more likely to experience complications from the flu [10]. Influenza can exacerbate existing conditions and lead to longer recovery times. Annual vaccination helps lower these risks and prevents disease flare-ups triggered by flu infection.
Healthcare Workers and Caregivers
Those who work in healthcare or provide care to vulnerable individuals, such as the elderly or chronically ill, are at increased risk of contracting and spreading influenza. Vaccinating this group not only protects them but also helps safeguard the health of the people they care for.
When’s the best time to get a flu vaccination?
There is no hard-and-fast rule when it comes to getting a flu vaccine. However, there are certain instances where it may be more beneficial for you, such as:
- Peaks in flu circulation — In Singapore, ideal times to get a flu vaccine would be in April, to protect against the mid-year spike, and October to protect you until the end of the year, when flu more commonly spreads.
- Before traveling — Getting a flu vaccination right before a trip can help prevent you from falling ill and putting a halt on your holiday.
- Before the school term starts — Schools are high-risk environments for flu transmission, and getting your child vaccinated ensures a good start to their school term, protecting them from infection.
- Before medical procedures — If you expect to be hospitalised or have a compromised immunity, getting a flu vaccination will be ideal for extra protection and optimal outcomes while you heal from your procedure.
Addressing Common Misconceptions
Despite widespread public health campaigns and scientific evidence, several misconceptions about the flu vaccine persist. These misunderstandings can discourage people from getting vaccinated; as a result, they may put themselves and others at risk. Here are some common myths associated with influenza vaccines.
“The Flu Vaccine Can Cause The Flu”
This is one of the most persistent myths. In reality, the flu vaccine used in Singapore contains inactivated (killed) viruses or fragments of the virus that cannot cause illness. These components are designed to trigger an immune response, which helps the body build protection without causing infection.
Some people may experience mild side effects after vaccination, such as a low-grade fever, fatigue, or soreness at the injection site, but these are signs that the immune system is responding to the vaccine, not symptoms of influenza. The flu vaccine cannot give you the flu.
“Healthy Individuals Don’t Need the Vaccine”
It’s a common belief that flu vaccination is only necessary for the elderly or people with chronic illnesses. While high-risk groups are more likely to experience severe complications, healthy individuals can still get infected and suffer from uncomfortable symptoms, time off work or school, and, in rare cases, complications like pneumonia.
Moreover, healthy individuals can transmit the virus to others, including family members or colleagues who may be more vulnerable. Vaccinating healthy people contributes to community protection and helps break the chain of transmission.
“Vaccination Is Unnecessary If It’s Not Flu Season”
Unlike temperate countries with clear flu seasons, Singapore experiences influenza activity throughout the year, with peaks typically seen from May to July and November to January. This makes it important to stay protected regardless of the time of year.
Waiting for a “flu season” in Singapore can lead to missed opportunities for prevention. As immunity builds about two weeks after vaccination, timely vaccination, before known peak periods or ahead of travel to countries experiencing seasonal outbreaks, is essential for effective protection.
Potential Side Effects and Safety
The flu vaccine has a strong safety track record and is generally well-tolerated. Still, knowing what to expect can help you feel more confident about your decision.
Common Side Effects
Most people experience no issues after their flu shot. If side effects do occur, they are usually mild and go away within a couple of days. These may include:
- A sore or slightly swollen area around the injection site
- Low-grade fever
- Mild fatigue or muscle aches
These are normal immune responses and a sign that your body is developing protection.
Rare Side Effects
Severe reactions to the flu vaccine are extremely rare. In isolated cases, people may have allergic responses, such as hives, swelling, or breathing difficulties, usually within minutes of the injection.
Our clinical team monitors every patient briefly after vaccination and is fully equipped to manage any adverse reaction safely and promptly.
Why Flu Vaccination Matters Now More Than Ever
At Ardennes Health, we offer seasonal influenza vaccinations as part of our commitment to preventive care for individuals and families.
Influenza continues to be a significant public health concern in Singapore, as it affects people across all age groups. With year-round flu activity and seasonal surges, the importance of annual vaccination cannot be overstated. The flu vaccine offers reliable protection — not only reducing your risk of falling ill but also helping to prevent severe complications, hospitalisations, and the spread of the virus to others.
If you are unsure about whether the flu vaccine is right for you, our medical team is here to provide clear, personalised guidance based on your health needs. Book an appointment (link to contact us page) with us today for a consultation.
References
- Flu measures. (22nd April 2008.). Ministry of Health. Retrieved April 7, 2025, from https://www.moh.gov.sg/newsroom/flu-measures/
- Drobnik, J., Pobrotyn, P., Witczak, I. T., Antczak, A., & Susło, R. (2021). Influenza as an important factor causing increased risk of patients’ deaths, excessive morbidity and prolonged hospital stays. Archives of Medical Science : AMS, 19(4), 941–951. https://doi.org/10.5114/aoms/138145
- Influenza vaccination services offered by community pharmacists under new sandbox initiative. (n.d.). Ministry of Health. Retrieved April 7, 2025, from https://www.moh.gov.sg/newsroom/influenza-vaccination-services-offered-by-community-pharmacists-under-new-sandbox-initiative/
- CDC. (2024, September 27). Types of influenza viruses. Influenza (Flu). https://www.cdc.gov/flu/about/viruses-types.html
- Protocols and enhanced screening measures to prevent cross-border spread of influenza into singapore. (6th March 2025). Ministry of Health. Retrieved April 7, 2025, from https://www.moh.gov.sg/newsroom/protocols-and-enhanced-screening-measures-to-prevent-cross-border-spread-of-influenza-into-singapore/
- Strengthening influenza vaccination policies and programmes. (n.d.). Retrieved April 7, 2025, from https://www.who.int/news/item/04-02-2025-strengthening-influenza-vaccination-policies-and-programmes
- Flu and older adults. (2022, June 14). National Institute on Aging. https://www.nia.nih.gov/health/flu/flu-and-older-adults
- CDC. (2024, September 26). Respiratory viruses and young children. Respiratory Illnesses. https://www.cdc.gov/respiratory-viruses/risk-factors/young-children.html
- Oseghale, O., Vlahos, R., O’Leary, J. J., Brooks, R. D., Brooks, D. A., Liong, S., & Selemidis, S. (2022). Influenza virus infection during pregnancy as a trigger of acute and chronic complications. Viruses, 14(12), 2729. https://doi.org/10.3390/v14122729
- American Lung Association. Flu symptoms and risk factors. Retrieved April 7, 2025, from https://www.lung.org/lung-health-diseases/lung-disease-lookup/influenza/symptoms-causes-and-risk
- Kim, T. H. (2014). Seasonal influenza and vaccine herd effect. Clinical and Experimental Vaccine Research, 3(2), 128–132. https://doi.org/10.7774/cevr.2014.3.2.128
Table of Contents

Hitting your 30s can feel like a bittersweet milestone. You are wiser, more confident, and likely juggling a whirlwind of responsibilities. But as life shifts gears, so does your body. This decade often marks the beginning of subtle changes in health — changes that, if caught early, can help you stay ahead of the curve for years to come. While it’s easy to get swept up in career goals, family life, or personal aspirations, taking a moment to prioritise your health can make all the difference.
Think of your 30s as the foundation-building phase for your long-term well-being. Just like you plan for the future in other aspects of life, regular health screenings are a proactive way to ensure your body is ready to support your ambitions. These screenings aren’t just about addressing current concerns — they are about prevention, early detection, and giving you peace of mind.
This guide provides an overview of the key health screenings to consider in your 30s, designed to help you prioritise your well-being.

1. General Health Screenings
As a doctor, one of the first things I tell my patients in their 30s is that this is the decade where prevention is key. Many health conditions, like hypertension, high cholesterol, and even diabetes, can develop silently during this time without any noticeable symptoms. That’s why regular health screenings are so crucial — they allow us to detect and address these issues early, often before they become serious.
When we talk about general health screenings, we are not just ticking boxes; we are creating a baseline for your health. For example, tests for blood pressure, cholesterol levels, and blood sugar help us identify risks for cardiovascular disease or diabetes. These are common conditions that, if caught early, can be managed effectively through lifestyle changes or medication.
Another thing to keep in mind is that your screening should be personalised. Family history, lifestyle factors, and even your work environment play a role in determining which tests are most relevant for you. For instance, if you have a family history of heart disease or diabetes, you should start screenings earlier or do them more frequently.
I always remind my patients that these check-ups aren’t just about finding problems — they are about creating a roadmap for better health. They give us a chance to talk about diet, exercise, and stress management, which are just as important as the numbers on a lab report.
2. Cardiovascular Health
In your 30s, I often notice patients starting to ask more questions about their heart health, and rightly so. This is the decade when the effects of years of habits — whether good or bad — begin to show. It’s not uncommon to see slightly elevated blood pressure or cholesterol levels during this time, often without any symptoms. That’s why I encourage regular check-ups and simple screenings to ensure we catch any changes early. These small steps can make a big difference in keeping your heart healthy and your future bright.
Blood Pressure Monitoring
Did you know high blood pressure, or hypertension, is often called the “silent killer”? ([1] It rarely shows symptoms until it has caused significant damage to your heart or other organs. Monitoring your blood pressure during routine check-ups can detect hypertension early, and allow timely intervention through lifestyle changes or medications. These simple screenings can prevent complications like heart disease or stroke.

Cholesterol Level Assessment
A lipid profile test is another essential screening in your 30s [2]. Elevated cholesterol, particularly LDL (bad cholesterol), can lead to plaque build-up in your arteries, which significantly increases the risk of heart attacks and strokes. If your cholesterol levels are higher than recommended, we can work together to develop a plan involving dietary changes, exercise routines, or medications to bring them under control.
Cardiac Screening Procedures at Ardennes Health
At Ardennes Health, we and our partner clinics offer a comprehensive range of cardiac screening procedures to evaluate your heart health thoroughly:
- Electrocardiogram (ECG): Records the heart’s electrical activity to detect conditions such as arrhythmias and ischaemia.
- Echocardiogram (ECHO): Provides detailed images of the heart’s structure and function, often used to assess the heart valves and chambers.
- 2D Echocardiography (2DE): Offers two-dimensional images of the heart, helping detect structural abnormalities.
- CT Angiogram: A non-invasive imaging test that visualises blood vessels to identify blockages or abnormalities in the arteries.
- Treadmill Exercise Test (TMX): Monitors heart activity during physical exertion to identify potential coronary artery diseases or other heart-related conditions.
Laboratory Investigations for Cardiac Risk
In addition to imaging tests, we recommend specific lab investigations to gain a comprehensive understanding of your cardiovascular health:
- Cardiac Risk Profile: Includes advanced markers like homocysteine, Apo A1, Apo B, and the Apo A1/B ratio [3].
- Diabetic Profile: Tests like HbA1c and fasting blood glucose to assess blood sugar levels, as diabetes is a significant risk factor for heart disease [4].
Whether you’re navigating a high-stress career, adjusting to parenthood, or simply working towards a healthier lifestyle, regular cardiac screenings are invaluable. These tests are not just for those with a family history of heart disease — they are for anyone who values their well-being. By prioritising these screenings now, you are building a solid foundation for a strong and healthy heart in the decades ahead.
3. Cancer Screenings
When it comes to cancer, early detection is your best defence. Many of my patients in their 30s ask whether it’s too soon to start thinking about cancer screenings. My answer is always the same: it’s never too early to prioritise your health, especially if you have a family history or other risk factors. Let me explain why these screenings matter and which ones you should consider.
Breast Cancer Screening
In your 30s, taking a proactive approach to breast health is essential, particularly if you have a family history of breast cancer or other risk factors. Routine mammograms are typically recommended starting at age 40 for women at average risk, but for those with a higher risk, earlier screenings may be necessary [5]. It’s always best to discuss your individual risk factors and screening plan with your healthcare provider.
For women in their 30s, breast ultrasounds can be a helpful option. This imaging technique uses sound waves to examine breast tissue and can detect abnormalities such as lumps or cysts. For those looking for additional and comprehensive screening methods, the Mastocheck Early Breast Cancer Screening is a valuable tool. This non-invasive blood test utilises proteomics-based early diagnostic technology to detect early-stage breast cancer. It’s particularly beneficial for women who may not yet need routine mammograms or who want an extra layer of reassurance.

Multi-Cancer Early Screening
Many people think cancer screenings are limited to specific types of cancer, but that’s no longer the case. With advancements in technology, we now have tests like LucenceINSIGHT that can screen for multiple cancers using a single blood sample. This test is a powerful tool for detecting cancers that are often asymptomatic in the early stages, such as pancreatic or ovarian cancer.
I recommend this test to anyone with a family history of cancer or to those who want a thorough evaluation of their health. LucenceINSIGHT helps us detect signals of cancer even when one is asymptomatic. This helps us detect issues early and act quickly, making it an excellent example of how modern medicine is transforming preventive care.
Cancer screenings aren’t about waiting for something to go wrong — they are about staying one step ahead. Whether it’s through a mammogram, Mastocheck, or LucenceINSIGHT, these tools help us identify risks early, giving you more options and better outcomes.
Summary
Entering your 30s is a turning point — a decade where proactive health choices can significantly shape your future well-being. By now, you have learned about the essential health screenings that address different aspects of your health: general health check-ups, cardiovascular assessments, and cancer screenings. But the key message is this: take action.
Health screenings aren’t just medical procedures; they are opportunities. Opportunities to catch silent health risks early, to make informed decisions, and to take preventive steps that can save you from future complications. This is your chance to build a foundation for a healthier, more resilient life — not just for yourself but for those who depend on you.
At Ardennes Health, we understand that taking the first step can sometimes feel overwhelming. That’s why we are here to make the process as efficient and supportive as possible. Whether it’s helping you choose the right screenings or guiding you through your results, our goal is to empower you to prioritise your health confidently. Schedule an appointment with us for your health screenings today.
References
- Research, C. for D. E. and. (2024). High blood pressure–understanding the silent killer. FDA. https://www.fda.gov/drugs/special-features/high-blood-pressure-understanding-silent-killer
- Lee, Y., & Siddiqui, W. J. (2025). Cholesterol levels. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK542294/
- Bodde, M. C., Hermans, M. P. J., Jukema, J. W., Schalij, M. J., Lijfering, W. M., Rosendaal, F. R., Romijn, F. P. H. T. M., Ruhaak, L. R., van der Laarse, A., & Cobbaert, C. M. (2019). Apolipoproteins A1, B, and apoB/apoA1 ratio are associated with first ST-segment elevation myocardial infarction but not with recurrent events during long-term follow-up. Clinical Research in Cardiology, 108(5), 520–538. https://doi.org/10.1007/s00392-018-1381-5
- Sherwani, S. I., Khan, H. A., Ekhzaimy, A., Masood, A., & Sakharkar, M. K. (2016). Significance of hba1c test in diagnosis and prognosis of diabetic patients. Biomarker Insights, 11, 95–104. https://doi.org/10.4137/BMI.S38440
- omlinson-Hansen, S. E., Budh, D. P., & Sapra, A. (2025). Breast cancer screening in the average-risk patient. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK556050/
Table of Contents
Health screenings are an important aspect of preventive healthcare, helping individuals detect potential issues early, manage existing conditions effectively, and maintain overall well-being. Health screenings are more than just routine check-ups—they are proactive steps toward a longer and healthier life.
In Singapore, common health issues include diabetes [1], cardiovascular diseases, and various types of cancer, several of which can be managed with early intervention. This guide will help you understand the types of health screenings that are relevant to you based on your age, gender, lifestyle, and risk factors.
Benefits of Regular Health Screenings
Regular screenings are vital for early detection and prevention. Beyond addressing physical health, these check-ups also provide peace of mind and the opportunity to make lifestyle changes and take better care of your health.
Here are some major benefits of regular health screenings:
- Early detection: Identifies diseases like diabetes, hypertension, or cancer before symptoms appear. This can improve the chances of successful treatment and recovery.
- Prevention of chronic health conditions: Health screenings enable timely intervention to prevent diseases from progressing into chronic conditions. It also helps people to understand their health and make lifestyle adjustments accordingly.
- Management of current conditions: Health screenings help individuals monitor their conditions and treatment so that they know they are taking the right steps, such as adjusting medications.
- Peace of mind and awareness: Regular health screenings help individuals alleviate their anxiety about perceived health problems and encourage proactive health management.

Health screenings, although general, are best tailored to each individual specifically depending on factors such as:
- Age
- Gender
- Family history
- Additional risk factors and concerns
This is why it’s important to book a consultation to evaluate each individual and their risk factors before recommending an appropriate health screening.
Health Screenings for Adults (General Recommendations)
Health screenings help adults stay ahead of health issues and challenges. Routine screenings give us valuable insights into our health and well-being, allowing us to detect and manage conditions such as high blood pressure and diabetes early. These tests offer a practical way to safeguard our health and make informed decisions.
Here are the general health screening recommendations for adults and their purposes:
- Blood Test: A general blood test assesses various components of the blood, such as red and white blood cell counts, haemoglobin, and platelets.
- Pressure Check: High blood pressure, or hypertension [2], is often called a “silent killer” because it usually presents no symptoms but significantly increases the risk of heart disease, stroke, and kidney failure. Regular blood pressure checks ensure early detection, allowing timely lifestyle changes or treatment to manage the condition and reduce long-term health risks.
- Cholesterol Test: A cholesterol test [3], or lipid profile, measures levels of good (HDL) and bad (LDL) cholesterol in the blood. High LDL or low HDL levels can lead to plaque buildup in arteries, increasing the risk of heart attacks and strokes. Regular monitoring helps to assess current cardiovascular health and encourages lifestyle and dietary changes.
- Blood Sugar Level Test: A blood sugar test evaluates glucose levels in the blood to detect prediabetes or diabetes. Early detection is critical for managing blood sugar and preventing complications such as nerve damage, kidney disease, and vision loss. Tests may include fasting blood sugar, HbA1c, or oral glucose tolerance tests.
- Body Mass Index (BMI) Measurement: The BMI test [4] measures body fat based on height and weight, indicating whether a person falls within a healthy weight range. It helps identify risks associated with obesity, such as diabetes, heart disease, and joint problems.
- Hepatitis Profile: This test screens for hepatitis viruses (A, B, and C), which can cause liver inflammation and damage.
- Renal Profile: The renal profile evaluates kidney function by measuring levels of creatinine, urea, and electrolytes like sodium and potassium in the blood. It also can detect kidney disease or dysfunction at an early stage.
- Thyroid Profile: This test measures thyroid hormone levels, including TSH, T3, and T4, to assess thyroid gland function and identify conditions like hypothyroidism or hyperthyroidism.
- Bone and joint screenings: Bone and joint screenings involve tests like bone density scans (DEXA) and assessments for inflammatory markers to evaluate bone strength and detect conditions like osteoporosis or arthritis.
- Tumor marker tests: These tests measure specific substances in the blood, urine, or tissues that may indicate the presence of certain types of cancer.
Preventive Cancer Screenings:
- Cervical Cancer: The Pap smear detects precancerous changes or abnormalities in the cervix, allowing early treatment before cancer develops. It is generally recommended for females aged 25-69.
- Breast Cancer: Mammograms use low-dose X-rays to detect breast cancer at an early stage before symptoms develop. Women aged 40 and older are recommended to undergo screenings every one to two years, depending on their risk factors and family history.
- Colorectal Cancer: Colorectal cancer screening involves tests like the faecal occult blood test (detecting hidden blood in stool) or colonoscopy (visual examination of the colon). These screenings identify early cancer or precancerous polyps.
- Prostate Cancer: The prostate-specific antigen (PSA) test measures PSA levels in the blood, which may indicate prostate cancer or other conditions like an enlarged prostate.
Other Essential Tests
- Liver and Kidney Function Tests: These blood tests evaluate the function of the liver and kidneys. They detect conditions like liver disease, hepatitis, or kidney damage, often before symptoms develop.
- Vision and Hearing Tests: Vision tests assess eye health and detect issues such as glaucoma, cataracts, or refractive errors. Hearing tests identify hearing loss, which is common with age or due to prolonged exposure to loud environments.

Health Screenings by Age
Health screenings are aligned with the specific needs of different age groups. In your 20s and 30s, baseline tests like blood pressure, cholesterol, and blood sugar assessments are typically recommended along with mental health screenings. In your 40s, more comprehensive screenings such as mammograms, Pap smears, and colonoscopies become crucial for detecting early signs of cancer. Women may also benefit from bone health assessments as hormonal changes begin to impact bone density.
In your 50s and beyond, screenings intensify to include heart health evaluations like stress tests and ECGs, as well as checks for dementia risk, vision, and hearing impairments. Tailoring screenings to your age ensures timely detection and intervention and contributes to more positive health outcomes.
Here are the recommended health screenings based on age groups:
| Age Group | Recommended Health Screenings |
| 30s – 40s | Cancer screenings (mammogram, Pap smear, colonoscopy)Bone health testsHormonal health checksSexually Transmitted Diseases (STD) checks |
| 40s – 50s | Cancer screenings (mammogram, Pap smear, colonoscopy)Bone health testsHormonal health checks |
| 50s and beyond | Frequent cancer screeningsHeart health tests (stress test, ECG)Dementia riskVision and hearing checks |
Health Screenings Based on Gender
Health screenings often vary by gender due to differences in anatomy, hormonal influences, and disease risks. While general tests such as blood tests and cholesterol checks are the same recommendations for both genders, other tests differ. For women, screenings often include reproductive and hormonal health, including Pap smears [5] for cervical cancer, mammograms for breast cancer, and bone density tests to monitor osteoporosis risk, particularly after menopause.
For men, health screenings may also include prostate cancer screenings (PSA tests) [6] and guidance on testicular self-examinations to help detect specific cancers early. Gender-specific screenings provide a comprehensive approach to maintaining health and addressing risks effectively.
Here are some recommended health screenings based on gender:
| Gender | Recommended Health Screenings |
| Women | Cervical Cancer Screening (Regular Pap smears)Breast Cancer Screening (Mammograms starting at age 40)Bone density testsPregnancy-related screeningsHormonal checks |
| Men | Prostate Cancer Screening (Men aged 50 and above).Cardiovascular Health CheckHormonal checks |

Health Screenings Based on Lifestyle, Risk Factors, and Specific Conditions
Your lifestyle and personal risk factors also influence the type of health screenings you need. Smokers, for example, should prioritise lung cancer screenings and respiratory function tests to detect potential damage early. If you have a family history of chronic diseases such as diabetes, heart disease, or cancer, genetic testing and enhanced cancer screenings can provide important insights. Sedentary lifestyles increase the risk of cardiovascular diseases and diabetes, making ECGs, stress tests, and blood sugar screenings essential.
If you already have a specific condition, you may also require additional health screenings. Here are some health screenings based on lifestyle and risk factors that you should consider:
| Lifestyle/Risk Factors | Recommended Health Screenings |
| Smokers | Lung cancer screeningRespiratory function testsCardiovascular health checkGeneral health screening |
| Family history of chronic diseases | Cancer screeningsCardiovascular health checkDiabetes screeningBone health assessmentGeneral health screening Kidney function test |
| Sedentary | Cardiovascular health checkGeneral health screeningMusculoskeletal assessmentsMental health screeningLiver and kidney function test |
| Specific condition | Chronic Illnesses: Lipid profile test Kidney Function tests Blood pressureDiabetes testLiver function testThyroid profile Heart Disease and Stroke Risk: ECG testEchocardiogramCholesterol levelsCT AngiogramLipoprotein(a)Homocysteine |

How to Choose a Health Screening Package in Singapore
Selecting the right health screening package in Singapore depends on your individual needs, budget, and preferences.
Private screening packages are also available for those seeking more comprehensive or personalised care. When choosing a private package, consider factors like the clinic’s reputation, the details of the tests included, and overall value for money. If you aren’t sure which health screening you should undergo, book a consultation with a doctor.
At Ardennes Health, we offer comprehensive health screening packages tailored to your needs and follow-up consultations to address any findings. Whether it’s preventive care or managing an existing condition, our team is here to guide you every step of the way.
Book your health screening with us at Ardennes Health or check out our packages here.
When to Seek Specialist Care
If your health screening results indicate abnormal findings, it’s important to seek medical advice as soon as possible. Abnormal results may signal underlying conditions that require further investigation. Based on the findings, your doctor may refer you to a specialist for a more in-depth evaluation and treatment. For example, if your screening suggests potential cancer, you may be referred to an oncologist, while abnormal heart test results may lead to a consultation with a cardiologist. Early intervention is crucial for managing health conditions effectively and improving long-term outcomes.
Conclusion
Regular health screenings are essential for everyone to stay aware of long-term health and proactive management of potential issues. Take charge of your health today by scheduling screenings tailored to your needs. If you’re still unsure which screening you should book, consult with our doctors to identify the most suitable options for you.
Frequently Asked Questions
What are the most important health screenings?
For most adults, important health screenings include body mass index (BMI), cholesterol and blood pressure screening, kidney function tests, tumour markers, and more. However, it depends on the individual and their lifestyle, age, and gender.
How often should I do health screening in Singapore?
The frequency of a health screening depends on various factors, including your age, gender, family history, and overall health status. For most adults, scheduling a comprehensive health screening every one to two years is an ideal approach to maintaining well-being. Consult with your doctor for more information.
Is health screening the same as medical check-up?
No, they are related but different. Health screenings are specific tests based on age, gender, or risk factors, while a medical check-up is a general examination by a doctor. Screenings are an important aspect of check-ups and help doctors gain a comprehensive understanding of your health to determine treatment or lifestyle changes.
References
- Channel NewsAsia. (2023, November 17). War against diabetes: Doctors seeing rise in patients below 40 due to lifestyle habits, early screening. Channel NewsAsia. Retrieved from: https://www.channelnewsasia.com/singapore/war-against-diabetes-singapore-doctors-seeing-rise-young-patients-below-40-lifestyle-habits-stress-early-screening-treatment-3921976
- Mayo Clinic. (n.d.). High blood pressure (hypertension) – Symptoms and causes. Mayo Clinic. Retrieved from https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/syc-20373410
- Cleveland Clinic. (n.d.). Cholesterol: Understanding levels & numbers. Cleveland Clinic. Retrieved from: https://my.clevelandclinic.org/health/articles/11920-cholesterol-numbers-what-do-they-mean
- Singapore Heart Foundation. (n.d.). BMI calculator. Singapore Heart Foundation. Retrieved from https://www.myheart.org.sg/tools-resources/bmi-calculator/
- Mayo Clinic. (n.d.). Pap smear: Overview. Mayo Clinic. Retrieved from https://www.mayoclinic.org/tests-procedures/pap-smear/about/pac-20394841
- Singapore Cancer Society. (n.d.). Prostate cancer. Singapore Cancer Society. Retrieved from https://www.singaporecancersociety.org.sg/learn-about-cancer/types-of-cancer/prostate-cancer.html
- Ministry of Health Singapore. (2024, December 2). Community Health Assist Scheme (CHAS). Ministry of Health. Retrieved from https://www.moh.gov.sg/managing-expenses/schemes-and-subsidies/chas
- Ministry of Health Singapore. (2024, December 2). Enhanced Screen for Life. Ministry of Health. Retrieved from https://www.moh.gov.sg/managing-expenses/schemes-and-subsidies/enhanced-screen-for-life
Breast cancer remains a significant health concern for women throughout the globe. In Singapore, it stands as the most common type of cancer among women. The Singapore Cancer Registry [1] reported that breast cancer accounts for nearly one in three cancer diagnoses among women in the country. This translates to 29.7% [2] of all female cancers, with approximately 1,100 new cases diagnosed annually. However, what is even more concerning is the fact that roughly 270 women [3] succumb to the disease each year.
Due to its prevalence, early detection through regular screening plays a critical role in improving the survival rate. In fact, research shows that early diagnosis can increase the chances of successful treatment by as much as 90% [4].
The aim of breast cancer screening is to identify the cancer at its earliest stage, ideally before symptoms are noticeable. By detecting cancer early, women have more treatment options available, and a greater likelihood of successful outcomes. This guide will provide a comprehensive overview of the breast cancer screening options available today, from blood tests to mammograms, and how each method can contribute to early detection.

Understanding Breast Cancer Screening
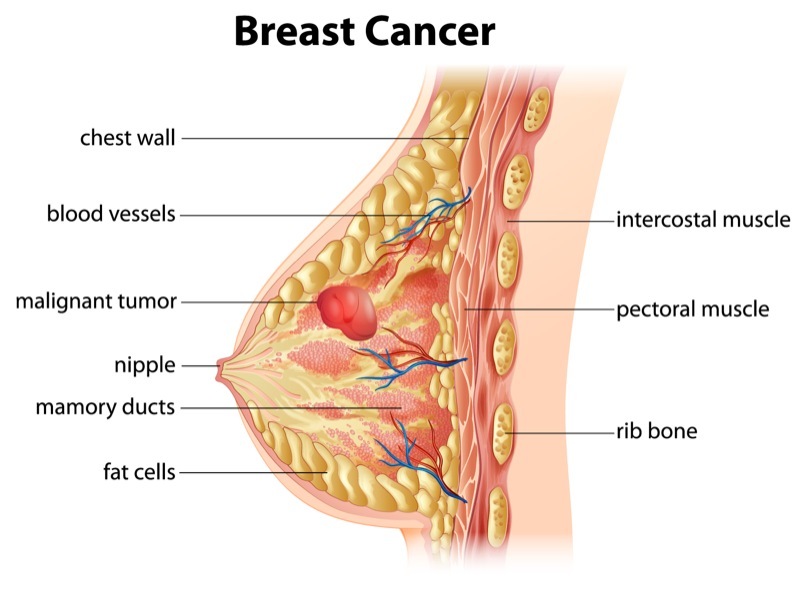
Breast cancer screening refers to the preventive measures taken to detect breast cancer before any symptoms emerge. Unlike diagnostic tests that are performed when there are visible signs, or symptoms of breast cancer, screening is done on seemingly healthy individuals, especially among those with a family history of breast cancer. The primary objective of screening is to identify cancer early, ideally when it is confined to the breast tissue, and has not spread to other parts of the body.
Regular breast cancer screening is essential for all women, particularly those over the age of 40 years old, or those with a family history of breast cancer. However, women with other high-risk factors as listed below may need to begin screening early:
- Age — as women age, the risk of breast cancer increases, with most cases diagnosed after the age of 50 [5].
- Dense breast — women with dense breasts [6] are more at risk of breast cancer, with the density making it harder to see tumours on a mammogram.
- Family history — a family history [8] of breast cancer increases the possibility of breast cancer.
- Genetics — inherited mutations to certain genes (BRCA1, and BRCA2 [9]) can increase the likelihood of developing breast cancer.
- Menstrual history — women who started menstruating before 12 years old, or started menopause after 55 years old are more at risk of developing breast cancer due to the long exposure to hormones [11].
- Previous breast cancer history — women with a previous history of breast cancer [12] are at risk of relapsing. Meanwhile, women with a history of benign breast diseases like lobular carcinoma in situ, or atypical ductal hyperplasia, are more prone to developing breast cancer.
- Previous radiation treatment — prior exposure to radiation [13] due to treatment to the chest, or breasts before 30 years old increases the risk of breast cancer.
- Alcohol consumption — a woman’s risk of developing breast cancer increases if she consumes alcohol at an excessive rate [14].
- Lifestyle — women who lead a sedentary, or not physically active lifestyle are at an increased risk of developing breast cancer.
- Weight — women who are considered overweight or obese [15] after going through menopause are more likely to develop breast cancer compared to those who maintain a healthy weight.

It is important to understand that consistent screening can significantly improve a woman’s chance of beating the cancer, as early detection may also include the following benefits:
- Early intervention and treatment
- More treatment options available
- Better outcomes and results
- Lowers the necessity for more aggressive treatments
- Higher quality of life post-recovery
- Reduces the mortality rate
Be that as it may, it is crucial to choose the appropriate screening method based on individual risk factors, age, and lifestyle. In fact, working closely with a licensed, and qualified medical practitioner will be advantageous, as they can help tailor a screening plan that best suits each woman’s needs.
Breast Cancer Screening Methods
There are various screening methods available today, each with its own unique benefits, and limitations. These include blood tests, imaging techniques like mammograms, ultrasounds, and magnetic resonance imaging (MRI) for those at high risk. While there are many options available, the choice of screening method often depends on the individual’s risk profile, and medical history. The following briefly describes each method:
- Self examination — self examination involves checking your own breasts for lumps, changes in breast size or shape, nipple discharge or discolouration.
- Clinical breast exams — clinical examinations are performed by a trained doctor, who will check for breast abnormalities or lumps.
- Blood tests — Conventional blood tests can be undergone to detect breast cancer markers, as well as innovative advancements, such as Mastocheck (link to service page), which identifies specific biomarkers linked to early-stage breast cancer for earlier detection.
- Imaging tests — Imaging tests, such as mammograms, ultrasounds and magnetic resonance imaging (MRIs).
Each method plays a different role in breast cancer detection, and often, a combination of these tests may be necessary for comprehensive screening.
Blood Tests

Blood tests are often used to detect early signs of breast cancer. These tests work by identifying specific proteins, or markers, that cancer cells release into the bloodstream. To give an example, markers like CA 15-3, and CEA can sometimes indicate the presence of cancer, although these markers are not exclusively specific to breast cancer.
Even so, blood tests are valued for their non-invasive nature. They can be conducted quickly, with results available in a shorter time frame compared to imaging techniques. However, while blood tests can provide valuable information, they are not typically used as standalone diagnostic tools. Their sensitivity, and specificity are limited, meaning that they are better suited as supplementary tests rather than primary screening tools.
That being said, blood tests are particularly useful for monitoring patients who have already been diagnosed with cancer to track the effectiveness of treatment, or detect recurrences. Be that as it may, as a screening tool, blood tests should be paired with other methods like imaging for a more accurate diagnosis.
The Role of Mastocheck in Early Screening
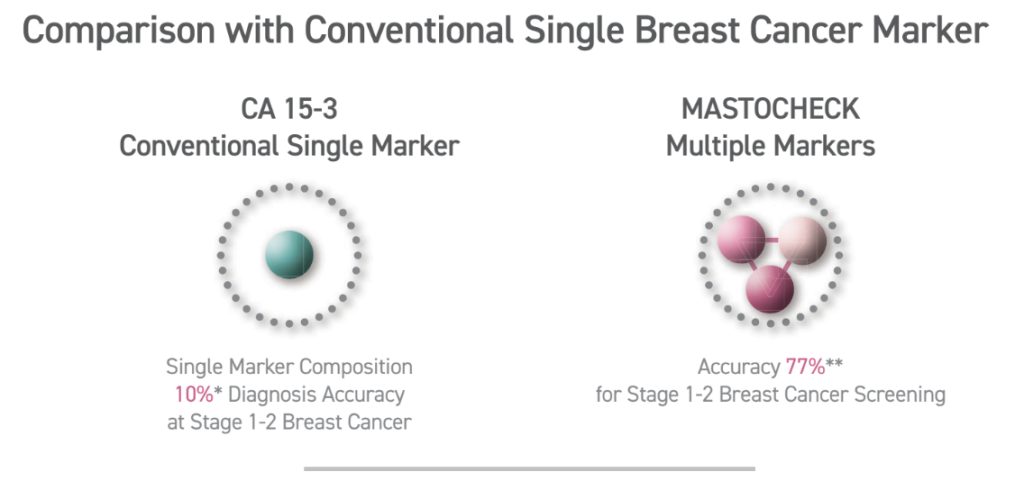
At Ardennes Healthcare, our Mastocheck Early Breast Cancer Screening (link to service page) is a blood test that analyses specific protein biomarkers that are indicative of breast cancer.
Unlike traditional blood tests that focus solely on inherited mutations, Mastocheck utilises advanced proteomic analysis to identify tumour-related proteins which are released by cancer cells and can serve as early indicators of tumour presence. This test is non-invasive, requiring only a blood sample, and can identify cancerous changes (disease-specific expression patterns) before they become visible through imaging. Hence, proteomics-based early diagnosis technology, like Mastocheck, greatly maximises diagnostic accuracy — with about 77% accuracy for stage 1-2 breast cancer.
However, it is essential to understand that while various blood tests can provide valuable insights into cancer risk, it is not a replacement for imaging techniques. Rather, it serves as a complementary tool, especially for those at higher risk of cancer (shows 10%-30% higher sensitivity compared to Mammography alone). Knowing your current cancer status through Mastocheck can help navigate the decision-making process regarding the frequency of follow-up screenings or the need for further diagnostic imaging.
The benefits of Mastocheck
The benefits of Mastocheck screening include:
- Early detection — Mastocheck enables the identification of breast cancer in its earliest stages, even before it becomes detectable through conventional imaging methods.
- Non-invasive procedure — Mastocheck only requires a small blood sample, offering a stress-free and comfortable screening process.
- High accuracy — It utilises advanced molecular diagnostic techniques, which allows it to detect specific cancer-related biomarkers, ensuring precise and reliable results.
- Enhanced detection for dense breasts — Mastocheck is especially effective for women with dense breast tissue where traditional mammograms may fall short in detecting. It delivers 10% – 30% greater sensitivity compared to a mammogram alone.
- Optimised outcomes — Early detection with Mastocheck increases the likelihood of successful treatment outcomes and reduces the need for more aggressive treatments.
- Radiation-free — By detecting cancer biomarkers without using radiation, Mastocheck provides a safer alternative for breast cancer screening.
- Accessibility — Suitable for younger women (ages 20 – 40), pregnant women, and those with breast implants or dense breast tissue.
Mammograms

Mammograms (link to service page) remain one of the most reliable screening tools for early breast cancer detection. This method involves using low-dose X-rays to examine breast tissue for any signs of tumours, or abnormal growths. For women aged 40, and above, regular mammograms are often recommended, as the risk of developing breast cancer increases with age.
A screening mammogram is typically done once every one to two years for women at average risk, while those at higher risk may need to undergo mammograms more frequently.
The benefits of mammograms are well-documented. In fact, they have been shown to reduce breast cancer mortality by enabling earlier diagnosis. However, some women may find the procedure uncomfortable due to the compression of breast tissue required for clear imaging. Additionally, mammograms do expose women to a small amount of radiation, but the risk is generally outweighed by the benefits of early detection.
Ultrasound and MRI: Complementary Tools

While mammograms are effective for most women, certain cases may require additional imaging techniques, like ultrasounds, and MRIs.
Ultrasound imaging (link to service page) is particularly useful for women with dense breast tissue, where mammograms may not be as effective. Dense tissue can obscure tumours, making them harder to detect. Ultrasound also works using sound waves to create images of the breast tissues, allowing for better visualisation of abnormalities that may not appear on a mammogram.
Meanwhile, MRI is an advanced imaging technique, typically for high-risk individuals. MRIs use magnetic fields, and radio waves to create detailed images of the breast, making it possible to detect cancers that might be missed by mammograms, or ultrasounds. In fact, women with a strong family history of breast cancer, or those with known genetic mutations like BRCA1, or BRCA2 may benefit from regular MRIs in addition to mammograms.
Both ultrasounds and MRIs serve as complementary tools to mammograms, and are usually recommended when additional clarity is needed.
A comprehensive approach: Mammogram with Mastocheck
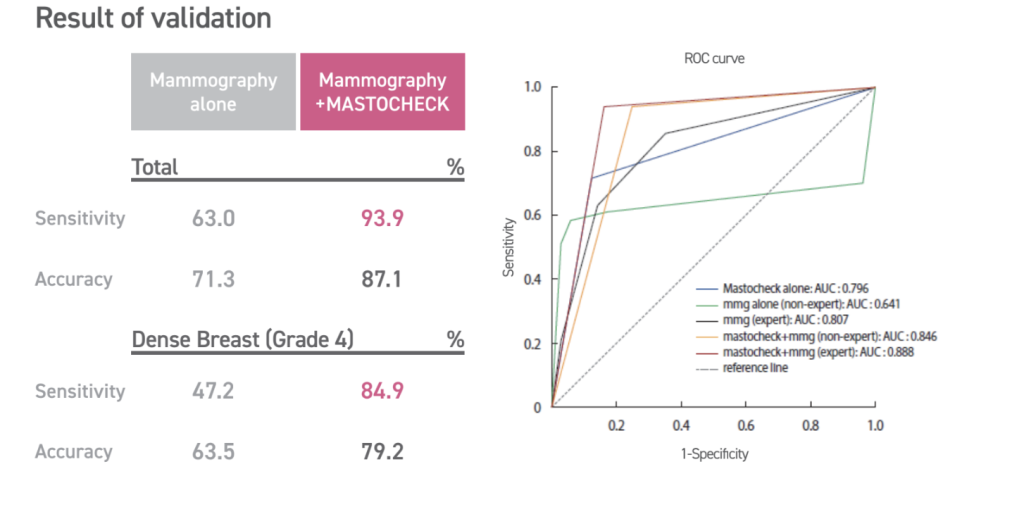
The importance of early detection in breast cancer
Early detection of breast cancer greatly improves survival rates and treatment outcomes. In fact, there is a 5-year relative survival rate for localised (tumour is confined to breast tissue) breast cancer is approximately 99%. This makes early detection of breast cancer and timely treatment paramount.
Why combine Mammogram and Mastocheck?
- Mastocheck — Mastocheck is a blood-based test that detects specific biomarkers linked to breast cancer, and offers 77% accuracy for stage 1-2 breast cancer screening. In contrast, conventional single marker CA15-3 offers an accuracy of 10%. In comparison, Mastocheck has a higher sensitivity and more accuracy in early-stage detection.
- Mammogram — A Mammogram is a widely used imaging test that plays an important role in breast cancer detection, and is highly effective at visualising microcalcifications and small masses and tumours in the breast that can indicate early-stage cancers. This makes it a reliable, non-invasive way to detect cancer early and improve treatment outcomes.
Combining a Mammogram with Mastocheck allows your doctor to detect structural changes in breast tissue and molecular changes in biomarkers that indicate early-stage breast cancer, offering a comprehensive significantly reducing the chances of false negatives.
Undergoing a Mastocheck blood test can also reduce your need for unnecessary procedures and additional stress. This is because it provides additional confirmation when ambiguous findings are detected via the mammogram, helping differentiate between the benign and malignant abnormalities in the breast.
What to Expect During a Breast Cancer Screening
We understand that undergoing breast cancer can be a daunting experience. At Ardennes Healthcare, we strive to help alleviate anxiety, and ensure you are well-prepared. Here, we break down the step-by-step for our general breast cancer screening procedures that are available at our healthcare facility.
Initial Consultation and Pre-Screening Assessment
Your breast cancer screening journey typically begins with an initial consultation with our general physician. During the consultation, our doctor will review your medical history, including any personal, or family history of breast cancer. They may ask about your lifestyle, any current symptoms you are experiencing, and other risk factors that may impact your screening plan. This consultation is essential as it ensures that the screening method chosen is appropriate for your specific risk profile.
Blood Tests (if applicable)
For those opting for blood tests like the Mastocheck screening, the procedure is straightforward and quick. Our nurse will draw a blood sample from a vein in your arm. The process typically takes less than 10 minutes, and is relatively painless, with only a minor prick sensation. The sample is then sent to a laboratory for analysis to detect potential cancer markers. While you are permitted to go home immediately after the procedure is done, results are generally available within a few days to a week.
Mammogram
If your screening includes a mammogram, you will be asked to change into a hospital gown, and remove any jewellery or clothing above the waist. Our technician will then position your breast on a flat surface, and gently compress it with a clear plastic plate. This compression is necessary to get a clear image of the breast tissue, and may cause some discomfort, but it only lasts for a few seconds. The technician will take images from different angles, usually two per breast. A simple mammogram process takes about 20 minutes to complete.
After the imaging is complete, the radiologist will review the images for any signs of abnormalities. It may take a few days for you to receive your results. In the event any suspicious findings are detected, further diagnostic tests may be recommended.
Ultrasound
For women with dense breast tissue, or if additional imaging is needed, an ultrasound may be recommended. During an ultrasound, you will lie down while a technician applies a gel to your breast. A handheld device called a transducer is moved over the area to capture images using sound waves. This procedure is painless and takes about 15 to 30 minutes.
Post-Screening Consultation
Once all of the tests are completed, you may have a follow-up consultation to discuss the results. If abnormalities are found, our doctor provider will guide you through the next steps, which may include additional diagnostic tests, biopsies, or further imaging to confirm the presence of cancer.

How to Prepare for Breast Cancer Screening
Being well-prepared can help ensure a smooth, and effective screening experience. To help you prepare for your breast screening, here is a detailed guideline to get you started.
Step 1: Scheduling Your Appointment
When scheduling an appointment for breast screening, do remember to pick a date at least a week after your menstrual period. This is due to the fact that your breasts are less likely to be tender during this time. Doing so can help minimise discomfort during the procedure. Additionally, for women undergoing blood tests or other non-imaging tests, there are no specific timing requirements.
Step 2: Dress Comfortably
On the day of your screening, wear a two-piece outfit so that you can easily remove your top piece of clothing for imaging procedures. Avoid wearing deodorant, antiperspirant, powders, or lotions on your underarms or breasts, as these products can show up on mammogram images as white spots, potentially leading to false alarms.
Step 3: What to Bring
It is important to bring your identification, health insurance information, and any prior imaging results if you have been screened before. Having these past records allows our doctors, and radiologists to compare images, and detect any subtle changes in breast tissue over time.
Step 4: Pain Management
If you are concerned about discomfort during a mammogram, consider taking an over-the-counter pain reliever, such as ibuprofen or acetaminophen, about an hour before your appointment. This can help alleviate any pain associated with breast compression. However, always speak with your doctor before taking any medication to prevent any complications.
Step 5: Preparing for an MRI
If you are scheduled for an MRI, inform the technician if you have any metal implants, pacemakers, or allergies, particularly to contrast dyes. You may need to fast for a few hours before the test if a contrast dye is being used. Additionally, do remember to remove any metal objects, such as jewellery, belts, or watches, before the scan, as this can disrupt the imaging process.
Step 6: Mental Preparation
For some women, the thought of undergoing a breast cancer screening can be anxiety-inducing, especially if it is their first time. But do remind yourself that these screenings are proactive steps toward maintaining your health, rather than dwelling on the possibility of malignancy. Some tips that can help ease your nerves before your appointment include deep breathing exercises, or listening to calming music. In fact, if asking questions can help reduce your anxiety, then do feel free to speak with our doctors to help you be more mentally prepared for the screening.
Step 7: Post-Screening Care
After your screening, there are generally no restrictions, and you can resume your normal activities immediately. However, if you experience any soreness after a mammogram, applying a cold compress can help reduce discomfort. For blood tests, keep the bandage on for a few hours to avoid bruises.
By following these preparation steps, and understanding what to expect, you can make your breast cancer screening experience as comfortable, and stress-free as possible.

Breast Cancer Screening Methods & Cost at a Glance
| Feature | Mammogram | Ultrasound | Mastocheck |
| Purpose | Standard screening for breast cancer. | Complements mammograms and can be used to evaluate dense breast tissue. | Blood test for early detection of specific biomarkers for breast cancer. |
| Recommended for | Women over the age of 40 years old or have risk factors for breast cancer. | Women with dense breasts, palpable lumps or other possible breast cancer indicators. | Early detection or supplemental screening. |
| Technology | X-ray imaging, may sometimes include a contrast for Contrast Enhanced Mammogram (CEM). | Utilises targeted ultrasound waves to visualise breast tissue structures. | Blood sample analysed for cancer markers. |
| Sensitivity | High sensitivity, but may not be as effective for dense breast tissue | High sensitivity, but may miss small or early cancers. | High sensitivity and provides risk indication for early cancers, but not the specific tumour location. Good early-warning tool. |
| Radiation exposure | Low-dose radiation. | None. | None. |
| Cost | From $99 | From $140 | From $170 |
Take Charge of Your Breast Health Today
Breast cancer screening is a powerful tool that can save lives by catching cancer early, often before any symptoms appear. However, deciding on the right screening plan is a highly personalised process that takes into account factors such as age, family history, genetic predisposition, and lifestyle. Understanding your options empowers you to make informed decisions about your health, and overall well-being.
For women in their 40s, annual mammograms are often recommended. However, younger women with elevated risk factors may benefit from additional testing options, such as Mastocheck, or breast ultrasounds. It goes without saying that consulting with a licensed, experienced physician is essential to developing a sound screening strategy tailored to your specific needs. A personalised plan not only maximises the effectiveness of early detection, but also offers peace of mind, knowing that you are taking proactive steps to protect your health.
At Ardennes Healthcare, we are dedicated to empowering women with comprehensive breast health services. We offer advanced screening options, including the Mastocheck test, to ensure you receive the best possible care. Our team is committed to providing personalised guidance every step of the way, helping you achieve optimal outcomes.
Remember, early detection is key. Take control of your breast health today! Schedule your screening appointment (link to contact us page) with us, and embark on a proactive journey toward wellness.
References
[1] Breast Cancer. (n.d.). In www.singaporecancersociety.org.sg. Retrieved November 14, 2024, from https://www.singaporecancersociety.org.sg/learn-about-cancer/types-of-cancer/breast-cancer.html
[2] [3] Jara-Lazaro, A. R., Thilagaratnam, S., & Tan, P. H. (2010). Breast cancer in Singapore: some perspectives. In Breast cancer (Tokyo, Japan) (Vol. 17, Issue 1, pp. 23–28). Breast cancer (Tokyo, Japan). https://doi.org/10.1007/s12282-009-0155-3
[4] By. (n.d.). The landscape of breast cancer screening and treatment in Singapore. In how well do we know it. Retrieved November 14, 2024, from https://www.singhealth.com.sg/news/medical-news-singhealth/landscape-breast-cancer-screening-treatment-singapore
[5] CDC. (2024). Breast Cancer Risk Factors. In Breast Cancer. https://www.cdc.gov/breast-cancer/risk-factors/index.html
[6] Dense Breasts: Answers to Commonly Asked Questions – NCI. (2018). In www.cancer.gov. https://www.cancer.gov/types/breast/breast-changes/dense-breasts
[7] Diethylstilbestrol (DES) Exposure and Cancer – NCI. (2021). In www.cancer.gov. https://www.cancer.gov/about-cancer/causes-prevention/risk/hormones/des-fact-sheet
[8] Brewer, H. R., Jones, M. E., Schoemaker, M. J., Ashworth, A., & Swerdlow, A. J. (2017). Family history and risk of breast cancer: an analysis accounting for family structure. In Breast cancer research and treatment (Vol. 165, Issue 1, pp. 193–200). Breast cancer research and treatment. https://doi.org/10.1007/s10549-017-4325-2
[9] Petrucelli N, Daly MB, Pal T. BRCA1- and BRCA2-Associated Hereditary Breast and Ovarian Cancer. 1998 Sep 4 [Updated 2023 Sep 21]. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1247/
[10] Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Collaborative Group on Hormonal Factors in Breast Cancer. (1997). Lancet (London, England), 350(9084), 1047–1059.
[11] Eaton L. (2002). Early periods and late childbearing increase risk of breast cancer, study confirms. BMJ : British Medical Journal, 324(7334), 386.
[12] Zeinomar, N., Phillips, K. A., Daly, M. B., Milne, R. L., Dite, G. S., MacInnis, R. J., Liao, Y., Kehm, R. D., Knight, J. A., Southey, M. C., Chung, W. K., Giles, G. G., McLachlan, S. A., Friedlander, M. L., Weideman, P. C., Glendon, G., Nesci, S., kConFab Investigators, Andrulis, I. L., Buys, S. S., … Terry, M. B. (2019). Benign breast disease increases breast cancer risk independent of underlying familial risk profile: Findings from a Prospective Family Study Cohort. International journal of cancer, 145(2), 370–379. https://doi.org/10.1002/ijc.32112
[13] Joshi, S. C., Khan, F. A., Pant, I., & Shukla, A. (2007). Role of radiotherapy in early breast cancer: an overview. International journal of health sciences, 1(2), 259–264.
[14] Liu, Y., Nguyen, N., & Colditz, G. A. (2015). Links between alcohol consumption and breast cancer: a look at the evidence. Women’s health (London, England), 11(1), 65–77. https://doi.org/10.2217/whe.14.62
[15] Dehesh, T., Fadaghi, S., Seyedi, M., Abolhadi, E., Ilaghi, M., Shams, P., Ajam, F., Mosleh-Shirazi, M. A., & Dehesh, P. (2023). The relation between obesity and breast cancer risk in women by considering menstruation status and geographical variations: a systematic review and meta-analysis. BMC women’s health, 23(1), 392. https://doi.org/10.1186/s12905-023-02543-5

